proteins
Nanoparticle Technology Holds Promise for Protecting Against Many Coronavirus Strains at Once
Posted on by Dr. Francis Collins

It’s truly encouraging to witness people all across our nation rolling up their sleeves to get their COVID-19 vaccines. That is our best chance to end this pandemic. But this is the third coronavirus to emerge and cause serious human illness in the last 20 years, and it’s probably not the last. So, this is also an opportunity to step up our efforts to develop vaccines to combat future strains of disease-causing coronavirus. With this in mind, I’m heartened by a new NIH-funded study showing the potential of a remarkably adaptable, nanoparticle-based approach to coronavirus vaccine development [1].
Both COVID-19 vaccines currently authorized for human use by the Food and Drug Administration (FDA) work by using mRNA to instruct our cells to make an essential portion of the spike protein of SARS-CoV-2, which is the novel coronavirus that causes COVID-19. As our immune system learns to recognize this protein fragment as foreign, it produces antibodies to attack SARS-CoV-2 and prevent COVID-19. What makes the new vaccine technology so powerful is that it raises the possibility of training the immune system to recognize not just one strain of coronavirus—but up to eight—with a single shot.
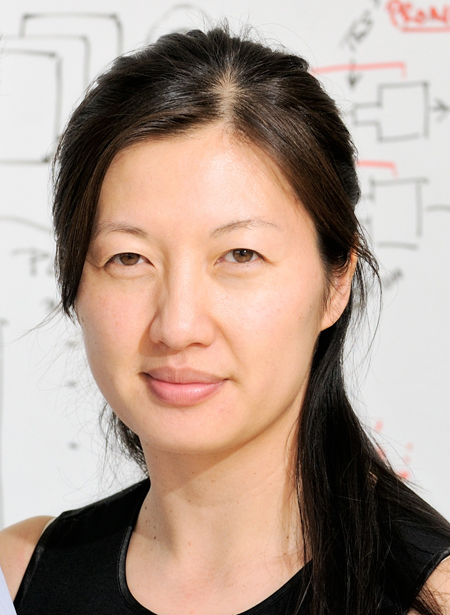
This approach has not yet been tested in people, but when a research team, led by Pamela Bjorkman, California Institute of Technology, Pasadena, injected this new type of vaccine into mice, it spurred the production of antibodies that react to a variety of different coronaviruses. In fact, some of the mouse antibodies proved to be reactive to related strains of coronavirus that weren’t even represented in the vaccine. These findings suggest that if presented with multiple different fragments of the spike protein’s receptor binding domain (RBD), which is what SARS-like coronaviruses use to infect human cells, the immune system may learn to recognize common features that might protect against as-yet unknown, newly emerging coronaviruses.
This new work, published in the journal Science, utilizes a technology called a mosaic nanoparticle vaccine platform [1]. Originally developed by collaborators at the University of Oxford, United Kingdom, the nanoparticle component of the platform is a “cage” made up of 60 identical proteins. Each of those proteins has a small protein tag that functions much like a piece of Velcro®. In their SARS-CoV-2 work, Bjorkman and her colleagues, including graduate student Alex A. Cohen, engineered multiple different fragments of the spike protein so each had its own Velcro-like tag. When mixed with the nanoparticle, the spike protein fragments stuck to the cage, resulting in a vaccine nanoparticle with spikes representing four to eight distinct coronavirus strains on its surface. In this instance, the researchers chose spike protein fragments from several different strains of SARS-CoV-2, as well as from other related bat coronaviruses thought to pose a threat to humans.
The researchers then injected the vaccine nanoparticles into mice and the results were encouraging. After inoculation, the mice began producing antibodies that could neutralize many different strains of coronavirus. In fact, while more study is needed to understand the mechanisms, the antibodies responded to coronavirus strains that weren’t even represented on the mosaic nanoparticle. Importantly, this broad antibody response came without apparent loss in the antibodies’ ability to respond to any one particular coronavirus strain.
The findings raise the exciting possibility that this new vaccine technology could provide protection against many coronavirus strains with a single shot. Of course, far more study is needed to explore how well such vaccines work to protect animals against infection, and whether they will prove to be safe and effective in people. There will also be significant challenges in scaling up manufacturing. Our goal is not to replace the mRNA COVID-19 vaccines that scientists developed at such a remarkable pace over the last year, but to provide much-needed vaccine strategies and tools to respond swiftly to the emerging coronavirus strains of the future.
As we double down on efforts to combat COVID-19, we must also come to grips with the fact that SARS-CoV-2 isn’t the first—and surely won’t be the last—novel coronavirus to cause disease in humans. With continued research and development of new technologies such as this one, the hope is that we will come out of this terrible pandemic better prepared for future infectious disease threats.
References:
[1] Mosaic RBD nanoparticles elicit neutralizing antibodies against SARS-CoV-2 and zoonotic coronaviruses. Cohen AA, Gnanapragasam PNP, Lee YE, Hoffman PR, Ou S, Kakutani LM, Keeffe JR, Barnes CO, Nussenzweig MC, Bjorkman PJ. Science. 2021 Jan 12.
Links:
COVID-19 Research (NIH)
Bjorkman Lab (California Institute of Technology, Pasadena)
NIH Support: National Institute of Allergy and Infectious Diseases
Deciphering Another Secret of Life
Posted on by Dr. Francis Collins
In 1953, Francis Crick famously told the surprised customers at the Eagle and Child pub in London that he and Jim Watson had discovered the secret of life. When NIH’s Marshall Nirenberg and his colleagues cracked the genetic code in 1961, it was called the solution to life’s greatest secret. Similarly, when the complete human genome sequence was revealed for the first time in 2003, commentators (including me) referred to this as the moment where the book of life for humans was revealed. But there are many more secrets of life that still need to be unlocked, including figuring out the biochemical rules of a protein shape-shifting phenomenon called allostery [1].
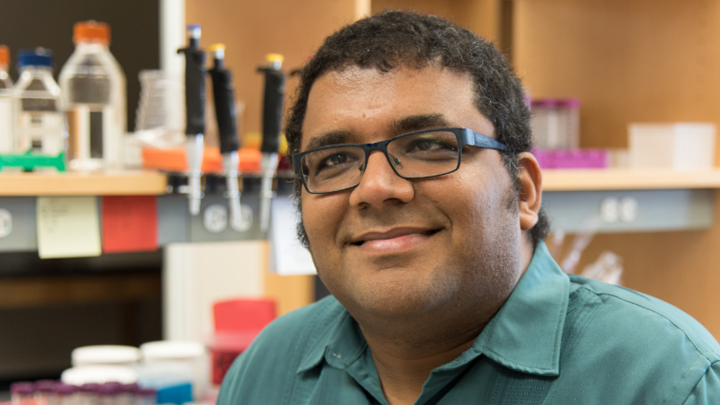
Among those taking on this ambitious challenge is a recipient of a 2018 NIH Director’s New Innovator Award, Srivatsan Raman of the University of Wisconsin-Madison. If successful, such efforts could revolutionize biology by helping us better understand how allosteric proteins reconfigure themselves in the right shapes at the right times to regulate cell signaling, metabolism, and many other important biological processes.
What exactly is an allosteric protein? Proteins have active, or orthosteric, sites that turn the proteins off or on when specific molecules bind to them. Some proteins also have less obvious regulatory, or allosteric, sites that indirectly affect the proteins’ activity when outside molecules bind to them. In many instances, allosteric binding triggers a change in the shape of the protein.
Allosteric proteins include oxygen-carrying hemoglobin and a variety of enzymes crucial to human health and development. In his work, Raman will start by studying a relatively simple bacterial protein, consisting of less than 200 amino acids, to understand the basics of how allostery works over time and space.
Raman, who is a synthetic biologist, got the idea for this project a few years ago while tinkering in the lab to modify an allosteric protein to bind new molecules. As part of the process, he and his team used a new technology called deep mutational scanning to study the functional consequences of removing individual amino acids from the protein [2].
The screen took them on a wild ride of unexpected functional changes, and a new research opportunity called out to him. He could combine this scanning technology with artificial intelligence and other cutting-edge imaging and computational tools to probe allosteric proteins more systematically in hopes of deciphering the basic molecular rules of allostery.
With the New Innovator Award, Raman’s group will first create a vast number of protein mutants to learn how best to determine the allosteric signaling pathway(s) within a protein. They want to dissect out the properties of each amino acid and determine which connect into a binding site and precisely how those linkages are formed. The researchers also want to know how the amino acids tend to configure into an inactive state and how that structure changes into an active state.
Based on these initial studies, the researchers will take the next step and use their dataset to predict where allosteric pathways are found in individual proteins. They will also try to figure out if allosteric signals are sent in one direction only or whether they can be bidirectional.
The experiments will be challenging, but Raman is confident that they will serve to build a more unified view of how allostery works. In fact, he hopes the data generated—and there will be a massive amount—will reveal novel sites to control or exploit allosteric signaling. Such information will not only expand fundamental biological understanding, but will accelerate efforts to discover new therapies for diseases, such as cancer, in which disruption of allosteric proteins plays a crucial role.
References:
[1] Allostery: an illustrated definition for the ‘second secret of life.’ Fenton AW. Trends Biochem Sci. 2008 Sep;33(9):420-425.
[2] Engineering an allosteric transcription factor to respond to new ligands. Taylor ND, Garruss AS, Moretti R, Chan S, Arbing MA, Cascio D, Rogers JK, Isaacs FJ, Kosuri S, Baker D, Fields S, Church GM, Raman S. Nat Methods. 2016 Feb;13(2):177-183.
Links:
Drug hunters explore allostery’s advantages. Jarvis LM, Chemical & Engineering News. 2019 March 10
Allostery: An Overview of Its History, Concepts, Methods, and Applications. Liu J, Nussinov R. PLoS Comput Biol. 2016 Jun 2;12(6):e1004966.
Srivatsan Raman (University of Wisconsin-Madison)
Raman Project Information (NIH RePORTER)
NIH Director’s New Innovator Award (Common Fund/NIH)
NIH Support: National Institute of General Medical Sciences; Common Fund
Happy New Year: Looking Back at 2016 Research Highlights
Posted on by Dr. Francis Collins
 Happy New Year! While everyone was busy getting ready for the holidays, the journal Science announced its annual compendium of scientific Breakthroughs of the Year. If you missed it, the winner for 2016 was the detection of gravitational waves—tiny ripples in the fabric of spacetime created by the collision of two black holes 1.3 billion years ago! It’s an incredible discovery, and one that Albert Einstein predicted a century ago.
Happy New Year! While everyone was busy getting ready for the holidays, the journal Science announced its annual compendium of scientific Breakthroughs of the Year. If you missed it, the winner for 2016 was the detection of gravitational waves—tiny ripples in the fabric of spacetime created by the collision of two black holes 1.3 billion years ago! It’s an incredible discovery, and one that Albert Einstein predicted a century ago.
Among the nine other advances that made the first cut for Breakthrough of the Year, several involved the biomedical sciences. As I’ve done in previous years (here and here), I’ll kick off this New Year by taking a quick look of some of the breakthroughs that directly involved NIH support:
Creative Minds: Breaking Size Barriers in Cryo-Electron Microscopy
Posted on by Dr. Francis Collins

Dmitry Lyumkis
When Dmitry Lyumkis headed off to graduate school at The Scripps Research Institute, La Jolla, CA, he had thoughts of becoming a synthetic chemist. But he soon found his calling in a nearby lab that imaged proteins using a technique known as single-particle cryo-electron microscopy (EM). Lyumkis was amazed that the team could take a purified protein, flash-freeze it in liquid nitrogen, and then fire electrons at the protein, capturing the resulting image with a special camera. Also amazing was the sophisticated computer software that analyzed the raw 2D camera images, merging the data and reconstructing it into 3D representations of the protein.
The work was profoundly complex, but Lyumkis thrives on solving extremely difficult puzzles. He joined the Scripps lab to become a structural biologist and a few years later used single-particle cryo-EM to help determine the atomic structure of a key protein on the surface of the human immunodeficiency virus (HIV), the cause of AIDS. The protein had been considered one of the greatest challenges in structural biology and a critical target in developing an AIDS vaccine [1].
Now, Lyumkis has plans to take single-particle cryo-EM to a whole new level—literally. He wants to develop new methods that allow it to model the atomic structures of much smaller proteins. Right now, single-particle cryo-EM has worked with proteins as small as roughly 150 kilodaltons, a measure of a protein’s molecular weight (the approximate average mass of a protein is 53 kDa). Lyumkis plans to drop that number well below 100 kDa, noting that if his new methods work as he hopes, there should be very little, if any, lower size limit to get the technique to work. He envisions generating within a matter of days or weeks the precise structure of an average-sized protein involved in a disease, and then potentially handing it off as an atomic model for drug developers to target for more effective treatment.
LabTV: Curious about Computer Modeling of Proteins
Posted on by Dr. Francis Collins
In many ways, Josh Carter is a typical college student, with a hectic schedule packed with classes and social activities. But when he enters a structural biology lab at Montana State University in Bozeman, Carter encounters an even faster paced world in which molecular interactions can be measured in femtoseconds—that is, 1 millionth of 1 billionth of 1 second.
Working under the expert eye of principal investigator Blake Wiedenheft, Carter is applying his computational skills to X-ray crystallography data to model the structures of various proteins, as well as to chart their evolution over time and map their highly dynamic interactions with other proteins and molecules. This basic science work is part of this NIH-funded lab’s larger mission to understand how bacteria defend themselves from the viruses that try to infect them. It’s a fascinating area of science with a wide range of potential applications, from treating diseases that arise from imbalances in the microbiome (the communities of microbes that live in and on our bodies) to developing new methods for gene editing and programmable control of gene expression.
Creative Minds: Mapping Molecules in their Cellular Compartments
Posted on by Dr. Francis Collins
If you were trying to understand how a city functions, it would be useful to map not only its streets and buildings, but to identify all of the people in the city and pinpoint their locations at different times throughout the day. That’s pretty much what biologists would like to do for a cell: map an entire living cell in a way that identifies all of its parts and shows their precise locations at various points in time.
The challenge has been developing the tools and technologies needed to create such a map. Among those who have risen to that challenge is Alice Ting, an associate professor at the Massachusetts Institute of Technology (MIT), Cambridge, MA, and winner of a 2008 NIH Director’s Pioneer Award and a 2013 NIH Director’s Transformative Research Award.
Snapshots of Life: Amyloid Glows in Polarized Light
Posted on by Dr. Francis Collins
While this may look like one of those bold canvases from the brush of an Abstract Expressionist, it’s actually a close-up of the biology underlying a rare, but relentless, group of conditions known as amyloidosis. This winner of the Federation of American Societies for Experimental Biology’s 2013 BioArt contest traces in exquisite detail the damage that amyloid, which is the abnormal accumulation of specific extracellular proteins, can inflict on the heart.
Next Page