smoking
10 Years of Protecting Public Health Through Tobacco Regulatory Research
Posted on by David M. Murray, Ph.D., NIH Office of Disease Prevention

“Kids are flocking to flavored, disposable e-cigarettes, study finds” – The Washington Post
“New ‘candy’ e-cigs catch fire after U.S. regulators stamp out Juul’s flavors” – Reuters
Headlines like these highlight a real challenge for people who want to protect kids from the harms of using tobacco products. While flavors, such as mint, menthol, watermelon, and apple pie are safe to consume in food products, inhaling them in tobacco products can be harmful and put the health of our kids at risk.+
A special kind of research is needed to help public health authorities keep up with the latest changes and trends in tobacco products. That includes studying how these flavored tobacco products are attractively marketed to children and how quickly many started using them.
In 2013, NIH and the Food and Drug Administration (FDA) launched a unique interagency partnership called the Tobacco Regulatory Science Program (TRSP), directed by Helen Meissner. It aims to reduce the public health impact of tobacco product use across the country. The NIH administers the research program through the Office of Disease Prevention (ODP), which I lead, to help inform FDA’s tobacco regulatory priorities.
This unique partnership also represents a new field of study called tobacco regulatory research. It informs proposed regulations for tobacco products based on strong scientific evidence. The TRSP brings together scientists from diverse fields, such as epidemiology, chemistry, toxicology, addiction, and psychology, to shed light on why people try and continue to use tobacco, how tobacco use affects health, and which policies might help reduce the risk of harm.
Now celebrating its 10th anniversary, this extremely productive partnership has resulted in more than 400 research grants, all peer-reviewed and designed to increase our understanding of existing and emerging tobacco products and their associated health risks.
Our research includes studies showing that menthol in cigarettes makes it easier to start smoking by reducing the harshness of tobacco [1]. People who smoke menthol cigarettes also show more signs of nicotine dependence and, therefore, are less likely to successfully quit. The research shows this is because menthol interacts with nicotine in the brain, making nicotine even more addictive.
Additionally, researchers have explored how marketing and promotion of menthol and flavored tobacco products have targeted Black and LGBTQ+ people, socioeconomically disadvantaged populations, and people with mental health challenges. These studies show that this direct marketing has contributed to the burden of tobacco-related disease among these groups and widened health inequities [2].
The TRSP also has a real-world impact on shaping tobacco policy. In April 2022, the program’s sponsored research was cited in FDA-proposed rules to prohibit menthol as a characterizing flavor in cigarettes and ban all characterizing flavors (other than tobacco) in cigars [3]. These tobacco product standards will have a huge impact on public health by reducing youth experimentation with products like cigarettes, cigars, and cigarillos and increasing the number of people who quit smoking.
Many jurisdictions have already banned flavored tobacco products. Through our partnership with the FDA, TRSP-funded researchers have started evaluating the impact of these policies on tobacco use and public health. The need for research continues as we seek to understand how new tobacco products affect people’s use, attitudes, and health.
However, tobacco products that have the potential to addict a new generation to nicotine continue to be marketed. For example, new products that use “ice-hybrid” flavors which combine cooling and fruity/sweet properties, such as raspberry ice, are being used more often than either fruity/sweet or menthol/mint among young adult e-cigarette users [4]. Illegally marketed, but novel, flavored oral nicotine products, such as gummies and pouches, also are gaining appeal among young people. The dynamic nature of the tobacco market emphasizes the importance of TRSP to support research on tobacco products, directly informing tobacco regulation.
The success of TRSP over the past 10 years demonstrates how establishing a research pipeline that directly informs regulation can lead to effective, evidence-based health policies. The high output of research on the effects of new and emerging tobacco products, such as the appeal and addictiveness of flavored e-cigarettes, provides FDA with data to inform regulatory actions. This partnership is truly helping regulators and policymakers turn scientific discovery into actions designed to protect public health.
References:
[1] Use of menthol cigarettes, smoking frequency, and nicotine dependence among US youth. Leas EC, Benmarhnia T, Strong DR, Pierce JP. JAMA Netw Open. 2022 Jun 1;5(6):e2217144.
[2] Menthol smoking and related health disparities. Centers for Disease Control and Prevention, June 27, 2022.
[3] FDA proposes rules prohibiting menthol cigarettes and flavored cigars to prevent youth initiation, significantly reduce tobacco-related disease and death. FDA News Release, April 28, 2022.
[4] ‘Ice’ flavoured e-cigarette use among young adults. Leventhal A, Dai H, Barrington-Trimis J, Sussman S. Tob Control. 2023 Jan;32(1):114-117.
Links:
Smokefree.gov (U.S. Department of Health and Human Services, Washington, D.C.)
Office of Disease Prevention (NIH)
Tobacco Regulatory Science Program (ODP)
Director’s Messages (ODP)
Note: Dr. Lawrence Tabak, who performs the duties of the NIH Director, has asked the heads of NIH’s Institutes, Centers, and Offices to contribute occasional guest posts to the blog to highlight some of the interesting science that they support and conduct. This is the 29th in the series of NIH guest posts that will run until a new permanent NIH director is in place.
Possible Explanation for Why Some People Get More Colds
Posted on by Dr. Francis Collins

Getty Images/yourstockbank
Colds are just an occasional nuisance for many folks, but some individuals seem to come down with them much more frequently. Now, NIH-funded researchers have uncovered some new clues as to why.
In their study, the researchers found that the cells that line our airways are quite adept at defending against cold-causing rhinoviruses. But there’s a tradeoff. When these cells are busy defending against tissue damage due to cigarette smoke, pollen, pollutants, and/or other airborne irritants, their ability to fend off such viruses is significantly reduced [1].
The new findings may open the door to better strategies for preventing the common cold, as well as other types of respiratory tract infections caused by non-flu viruses. Even small improvements in prevention could have big implications for our nation’s health and economy. Every year, Americans come down with more than 500 million colds and similar infections, leading to reduced work productivity, medical expenses, and other costs approaching $40 billion [2].
Widening Gap in U.S. Life Expectancy
Posted on by Dr. Francis Collins
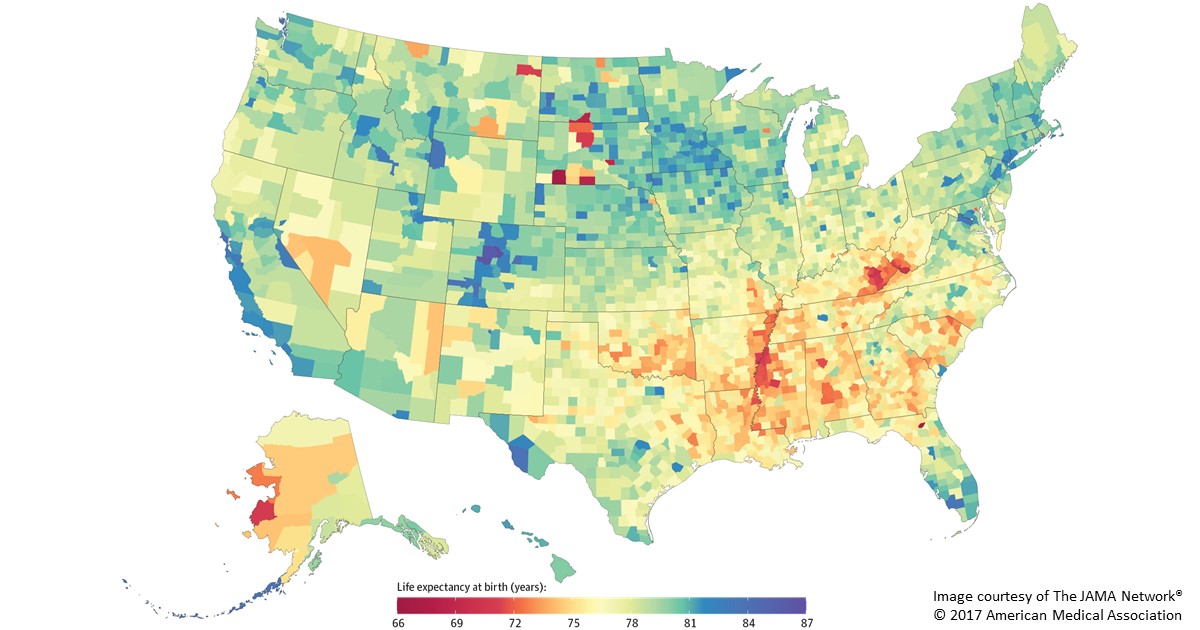
Caption: Life expectancy at birth by county, 2014. Life expectancy into 80s (blue), 70s (green, yellow, orange), 60s (red).
Americans are living longer than ever before, thanks in large part to NIH-supported research. But a new, heavily publicized study shows that recent gains in longevity aren’t being enjoyed equally in all corners of the United States. In fact, depending on where you live in this great country, life expectancy can vary more than 20 years—a surprisingly wide gap that has widened significantly in recent decades.
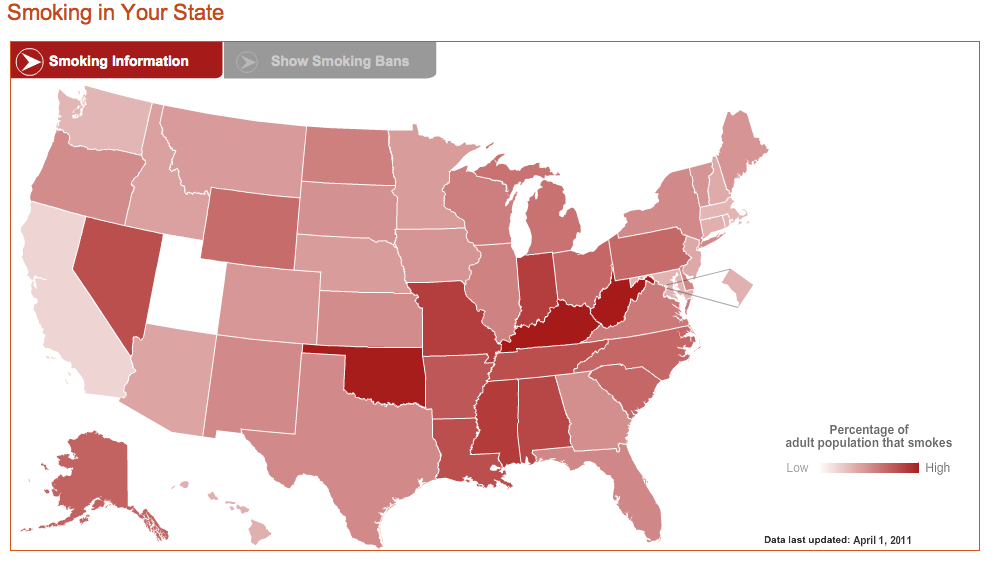
Researchers attribute this disturbing gap to a variety of social and economic influences, as well as differences in modifiable behavioral and lifestyle factors, such as obesity, inactivity, and tobacco use. The findings serve as a sobering reminder that, despite the considerable progress made possible by biomedical science, more research is needed to figure out better ways of addressing health disparities and improving life expectancy for all Americans.
In the new study published in JAMA Internal Medicine, a research team, partially funded by NIH, found that the average American baby born in 2014 can expect to live to about age 79 [1]. That’s up from a national average of about 73 in 1980 and around 68 in 1950. However, babies born in 2014 in remote Oglala Lakota County, SD, home to the Pine Ridge Indian Reservation, can expect to live only about 66 years. That’s in stark contrast to a child born about 400 miles away in Summit County, CO, where life expectancy at birth now exceeds age 86.
Are E-cigarettes Leading More Kids to Smoke?
Posted on by Dr. Francis Collins

Thinkstock\MilknCoffee
Today, thanks to decades of educational efforts about the serious health consequences of inhaled tobacco, fewer young people than ever smoke cigarettes in the United States. So, it’s interesting that a growing of number of middle and high school kids are using e-cigarettes—electronic devices that vaporize flavored liquid that generally contains nicotine.
E-cigarettes come with their own health risks, including lung inflammation, asthma, and respiratory infections. But their supporters argue that “vaping,” as it’s often called, might provide an option that would help young people steer clear of traditional cigarettes and the attendant future risks of lung cancer, emphysema, heart disease, and other serious health conditions. Now, a new NIH-funded study finds that this is—pardon the pun—mostly a pipe dream.
Analyzing the self-reported smoking behaviors of thousands of schoolkids nationwide, researchers found no evidence that the availability of e-cigarettes has served to accelerate the decline in youth smoking. In fact, the researchers concluded the opposite: the popularity of e-cigarettes has led more kids—not fewer—to get hooked on nicotine, which meets all criteria for being an addictive substance.
Study Finds No Safe Level of Smoking
Posted on by Dr. Francis Collins

Thinkstock\Nastco
Many Americans who’ve smoked cigarettes have been successful in their efforts to quit. But there’s some bad news for those who’ve settled for just cutting back: new evidence shows there’s no safe amount of smoking. One cigarette a day, or even less than that, still poses significant risks to your health.
A study conducted by NIH researchers of more than 290,000 adults between the ages of 59 and 82 found that those who reported smoking less than one cigarette per day, on average, for most of their lives were nine times more likely to die from lung cancer than those who never smoked. The outlook was even worse for those who smoked between one and 10 cigarettes a day. Compared to never-smokers, they faced a 12 times greater risk of dying from lung cancer and 1½ times greater risk of dying of cardiovascular disease.
Largest Study Yet Shows Mother’s Smoking Changes Baby’s Epigenome
Posted on by Dr. Francis Collins

Credit: Daniel Berehulak/Getty Images
Despite years of public health campaigns warning of the dangers of smoking when pregnant, many women are unaware of the risk or find themselves unable to quit. As a result, far too many babies are still being exposed in the womb to toxins that enter their mothers’ bloodstreams when they inhale cigarette smoke. Among the many infant and child health problems that have been linked to maternal smoking are premature birth, low birth weight, asthma, reduced lung function, sudden infant death syndrome (SIDS), and cleft lip and/or palate.
Now, a large international study involving NIH-supported researchers provides a biological mechanism that may explain how exposure to cigarette toxins during fetal development can produce these health problems [1]. That evidence centers on the impact of the toxins on the epigenome of the infant’s body tissues. The epigenome refers to chemical modifications of DNA (particularly methylation of cytosines), as well as proteins that bind to DNA and affect its function. The genome of an individual is the same in all cells of their body, but the epigenome determines whether genes are turned on or off in particular cells. The study found significant differences between the epigenetic patterns of babies born to women who smoked during pregnancy and those born to non-smokers, with many of the differences affecting genes known to play key roles in the development of the lungs, face, and nervous system.
Got Your Red On?
Posted on by Dr. Francis Collins
The hard truth is that heart disease is the #1 killer of American women. And it’s largely preventable. The Heart Truth® was started here at NIH’s National Heart, Lung, and Blood Institute to raise awareness of these truths. You’re probably most familiar with the campaign through its February 1st fashion statement, which has arguably become a cultural icon: the red dress. The Red Dress® is a decade old this year. And, like heart disease, it doesn’t discriminate by gender. Everyone can wear red today. It’s a symbol of solidarity – and a reminder that we should each attend to our heart’s needs every day: by making healthful decisions like exercising more, quitting smoking, and maintaining a healthy weight and blood pressure.
For more information:
The Heart Truth: http://www.nhlbi.nih.gov/educational/hearttruth/
Women and Heart Disease: http://www.nhlbi.nih.gov/health/health-topics/topics/hdw/

Click on the image to view full sized.
Source: National Heart, Lung, and Blood Institute, NIH
Smoking: It’s Killing Us
Posted on by Dr. Francis Collins
Smoking harms just about every body part—from heart and lungs to bladder and blood vessels. What’s new is that smoking is more of a health hazard than we thought. Two new, NIH-funded reports make the persuasive, and alarming, case—on average, smoking takes an entire decade off of your life! But smokers take note: there are tremendous benefits from quitting, regardless of your age.
