BBB
Childhood Cancer: Novel Nanoparticle Shows Early Promise for Brain Tumor
Posted on by Lawrence Tabak, D.D.S., Ph.D.
The human brain is profoundly complex, consisting of tens of billions of neurons that form trillions of interconnections. This complex neural wiring that allows us to think, feel, move, and act is surrounded by what’s called the blood-brain barrier (BBB), a dense sheet of cells and blood vessels. The BBB blocks dangerous toxins and infectious agents from entering the brain, while allowing nutrients and other essential small molecules to pass right through.
This gatekeeping function helps to keep the brain healthy, but not when the barrier prevents potentially life-saving drugs from reaching aggressive, inoperable brain tumors. Now, an NIH-funded team reporting in the journal Nature Materials describes a promising new way to ferry cancer drugs across the BBB and reach the sites of disease [1]. While the researchers have not yet tried this new approach in people, they have some encouraging evidence from studies in mouse models of medulloblastoma, an aggressive brain cancer that’s diagnosed in hundreds of children each year.
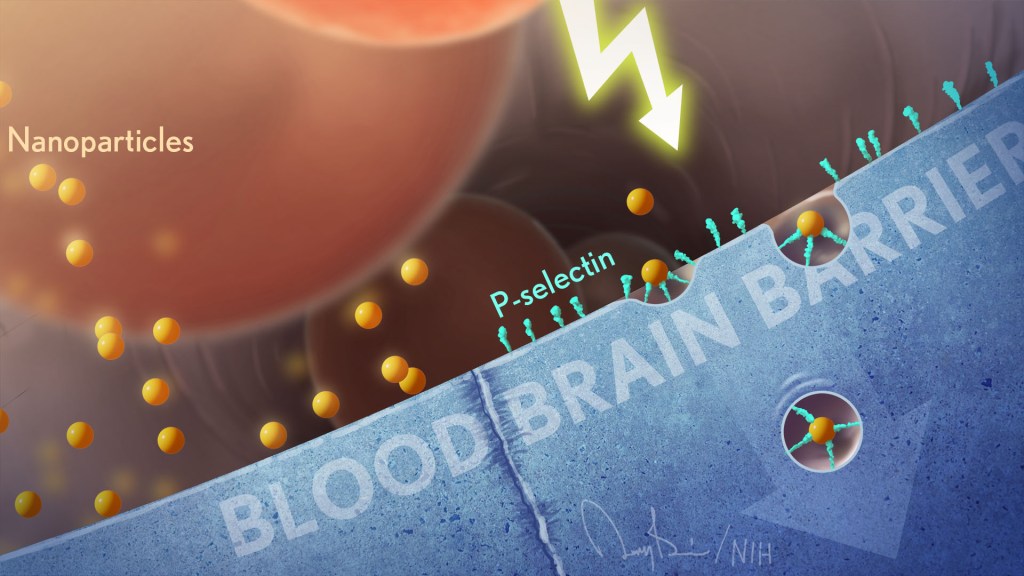
The team, including Daniel Heller, Memorial Sloan Kettering Cancer Center, New York, NY, and Praveen Raju, Icahn School of Medicine at Mount Sinai, New York, NY, wanted to target a protein called P-selectin. The protein is found on blood vessel cells at sites of infection, injury, or inflammation, including cancers. The immune system uses such proteins to direct immune cells to the places where they are needed, allowing them to exit the bloodstream and enter other tissues.
Heller’s team thought they could take advantage of P-selectin and its molecular homing properties as a potential way to deliver cancer drugs to patients. But first they needed to package the drugs in particles tiny enough to stick to P-selectin like an immune cell.
That’s when they turned to a drug-delivery construct called a nanoparticle, which can have diameters a thousand times smaller than that of a human hair. But what’s pretty unique here is the nanoparticles are made from chains of sugar molecules called fucoidan, which are readily extracted from a type of brown seaweed that grows in Japan. It turns out that this unlikely ingredient has a special ability to attract P-selectin.
In the new study, the researchers decided to put their novel fucoidan nanoparticles to the test in the brain, while building on their previous animal work in the lungs [2]. That work showed that when fucoidan nanoparticles bind to P-selectin, they trigger a process that shuttles them across blood vessel walls.
This natural mechanism should also allow nanoparticle-packaged substances in the bloodstream to pass through vessel walls in the BBB and into the surrounding brain tissue. The hope was it would do so without damaging the BBB, a critical step for improving the treatment of brain tumors.
In studies with mouse models of medulloblastoma, the team loaded the nanoparticles with a cancer drug called vismodegib. This drug is approved for certain skin cancers and has been tested for medulloblastoma. The trouble is that the drug on its own comes with significant side effects in children at doses needed to effectively treat this brain cancer.
The researchers found that the vismodegib-loaded nanoparticles circulating in the mice could indeed pass through the intact BBB and into the brain. They further found that the particles accumulated at the site of the medulloblastoma tumors, where P-selectin was most abundant, and not in other healthy parts of the brain. In the mice, the approach allowed the vismodegib treatment to work better against the cancer and at lower doses with fewer side effects.
This raised another possibility. Radiation is a standard therapy for children and adults with brain tumors. The researcher found that radiation boosts P-selectin levels specifically in tumors. The finding suggests that radiation targeting specific parts of the brain prior to nanoparticle treatment could make it even more effective. It also may help to further limit the amount of cancer-fighting drug that reaches healthy brain cells and other parts of the body.
The fucoidan nanoparticles could, in theory, deliver many different drugs to the brain. The researchers note their promise for treating brain tumors of all types, including those that spread to the brain from other parts of the body. While much more work is needed, these seaweed-based nanoparticles may also help in delivering drugs to a wide range of other brain conditions, such as multiple sclerosis, stroke, and focal epilepsy, in which seizures arise from a specific part of the brain. It’s a discovery that brings new meaning to the familiar adage that good things come in small packages.
References:
[1] P-selectin-targeted nanocarriers induce active crossing of the blood-brain barrier via caveolin-1-dependent transcytosis. Tylawsky DE, Kiguchi H, Vaynshteyn J, Gerwin J, Shah J, Islam T, Boyer JA, Boué DR, Snuderl M, Greenblatt MB, Shamay Y, Raju GP, Heller DA. Nat Mater. 2023 Mar;22(3):391-399.
[2] P-selectin is a nanotherapeutic delivery target in the tumor microenvironment. Shamay Y, Elkabets M, Li H, Shah J, Brook S, Wang F, Adler K, Baut E, Scaltriti M, Jena PV, Gardner EE, Poirier JT, Rudin CM, Baselga J, Haimovitz-Friedman A, Heller DA. Sci Transl Med. 2016 Jun 29;8(345):345ra87.
Links:
Medulloblastoma Diagnosis and Treatment (National Cancer Institute/NIH)
Brain Basics: Know Your Brain (National Institute of Neurological Disorders and Stroke/NIH)
The Daniel Heller Lab (Memorial Sloan Kettering Cancer Center, New York, NY)
Praveen Raju (Mount Sinai, New York, NY)
NIH Support: National Cancer Institute; National Institute of Neurological Disorders and Stroke
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Posted In: News
Tags: BBB, blood-brain barrier, brain, cancer, chemotherapy, childhood brain cancer, drug delivery, focal epilepsy, fucoidan, immune cells, inflammation, medulloblastoma, mouse model, multiple sclerosis, nanoparticles, nanotechnology, P-selectin, radiation oncology, seaweed, stroke, vismodegib
Making Personalized Blood-Brain Barriers in a Dish
Posted on by Dr. Francis Collins

The blood-brain barrier, or BBB, is a dense sheet of cells that surrounds most of the brain’s blood vessels. The BBB’s tiny gaps let vital small molecules, such as oxygen and water, diffuse from the bloodstream into the brain while helping to keep out larger, impermeable foreign substances that don’t belong there.
But in people with certain neurological disorders—such as amyotrophic lateral sclerosis (ALS) and Huntington’s disease—abnormalities in this barrier may block the entry of biomolecules essential to healthy brain activity. The BBB also makes it difficult for needed therapies to reach their target in the brain.
To help look for solutions to these and other problems, researchers can now grow human blood-brain barriers on a chip like the one pictured above. The high-magnification image reveals some of the BBB’s cellular parts. There are endothelial-like cells (magenta), which are similar to those that line the small vessels surrounding the brain. In close association are supportive brain cells known as astrocytes (green), which help to regulate blood flow.
While similar organ chips have been created before, what sets apart this new BBB chip is its use of induced pluripotent stem cell (iPSC) technology combined with advanced chip engineering. The iPSCs, derived in this case from blood samples, make it possible to produce a living model of anyone’s unique BBB on demand.
The researchers, led by Clive Svendsen, Cedars-Sinai, Los Angeles, first use a biochemical recipe to coax a person’s white blood cells to become iPSCs. At this point, the iPSCs are capable of producing any other cell type. But the Svendsen team follows two different recipes to direct those iPSCs to differentiate into endothelial and neural cells needed to model the BBB.
Also making this BBB platform unique is its use of a sophisticated microfluidic chip, produced by Boston-based Emulate, Inc. The chip mimics conditions inside the human body, allowing the blood-brain barrier to function much as it would in a person.
The channels enable researchers to flow cerebral spinal fluid (CSF) through one side and blood through the other to create the fully functional model tissue. The BBB chips also show electrical resistance and permeability just as would be expected in a person. The model BBBs are even able to block the entry of certain drugs!
As described in Cell Stem Cell, the researchers have already created BBB chips using iPSCs from a person with Huntington’s disease and another from an individual with a rare congenital disorder called Allan-Herndon-Dudley syndrome, an inherited disorder of brain development.
In the near term, his team has plans to model ALS and Parkinson’s disease on the BBB chips. Because these chips hold the promise of modeling the human BBB more precisely than animal models, they may accelerate studies of potentially promising new drugs. Svendsen suggests that individuals with neurological conditions might one day have their own BBB chips made on demand to help in selecting the best-available therapeutic options for them. Now that’s a future we’d all like to see.
Reference:
[1] Human iPSC-Derived Blood-Brain Barrier Chips Enable Disease Modeling and Personalized Medicine Applications. Vatine GD, Barrile R, Workman MJ, Sances S, Barriga BK, Rahnama M, Barthakur S, Kasendra M, Lucchesi C, Kerns J, Wen N, Spivia WR, Chen Z, Van Eyk J, Svendsen CN. Cell Stem Cell. 2019 Jun 6;24(6):995-1005.e6.
Links:
Tissue Chip for Drug Screening (National Center for Advancing Translational Sciences/NIH)
Stem Cell Information (NIH)
Svendsen Lab (Cedars-Sinai, Los Angeles)
NIH Support: National Institute of Neurological Disorders and Stroke; National Center for Advancing Translational Sciences
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Posted In: Snapshots of Life
Tags: Allan-Herndon-Dudley syndrome, ALS, amyotrophic lateral sclerosis, astrocytes, BBB, blood, blood vessels, blood-brain barrier, brain, CSF, Emulate, endothelial cells, Huntington's disease, iPSCs, microfluidics, neurological disorders, neurology, organoid, Parkinson's disease, precision medicine, rare disease, tissue chips
