microbiota
Targeting the Microbiome to Treat Malnutrition
Posted on by Dr. Francis Collins

Credit: International Centre for Diarrhoeal Disease Research, Bangladesh
A few years ago, researchers discovered that abnormalities in microbial communities, or microbiomes, in the intestine appear to contribute to childhood malnutrition. Now comes word that this discovery is being translated into action, with a new study showing that foods formulated to repair the “gut microbiome” may help malnourished kids rebuild their health [1].
In a month-long clinical trial in Bangladesh, 63 children received either regular foods to treat malnutrition or alternative formulations for needed calories and nutrition that also encouraged growth of beneficial microbes in the intestines. The kids who ate the microbiome-friendly diets showed improvements in their microbiome, which helps to extract and metabolize nutrients in our food to help the body grow. They also had significant improvements in key blood proteins associated with bone growth, brain development, immunity, and metabolism; those who ate standard therapeutic food did not experience the same benefit.
Globally, malnutrition affects an estimated 238 million children under the age 5, stunting their normal growth, compromising their health, and limiting their mental development [2]. Malnutrition can arise not only from a shortage of food but from dietary imbalances that don’t satisfy the body’s need for essential nutrients. Far too often, especially in impoverished areas, the condition can turn extremely severe and deadly. And the long term effects on intellectual development can limit the ability of a country’s citizens to lift themselves out of poverty.
Jeffrey Gordon, Washington University School of Medicine in St. Louis, and his NIH-supported research team have spent decades studying what constitutes a normal microbiome and how changes can affect health and disease. Their seminal studies have revealed that severely malnourished kids have “immature” microbiomes that don’t develop in the intestine like the microbial communities seen in well nourished, healthy children of the same age.
Gordon and team have also found that this microbial immaturity doesn’t resolve when kids consume the usual supplemental foods [3]. In another study, they turned to mice raised under sterile conditions and with no microbes of their own to demonstrate this cause and effect. The researchers colonized the intestines of the germ-free mice with microbes from malnourished children, and the rodents developed similar abnormalities in weight gain, bone growth, and metabolism [4].
All of this evidence raised a vital question: Could the right combination of foods “mature” the microbiome and help to steer malnourished children toward a healthier state?
To get the answer, Gordon and his colleagues at the International Centre for Diarrhoeal Disease Research, Dhaka, Bangladesh, led by Tahmeed Ahmed, first had to formulate the right, microbiome-friendly food supplements, and that led to some interesting science. They carefully characterized over time the immature microbiomes found in Bangladeshi children treated for severe malnutrition. This allowed them to test their new method for analyzing how individual microbial species fluctuate over time and in relationship to one another in the intestine [5]. The team then paired up these data with measurements of a set of more than 1,300 blood proteins from the children that provide “readouts” of their biological state.
Their investigation identified a network of 15 bacterial species that consistently interact in the gut microbiomes of Bangladeshi children. This network became their means to characterize sensitively and accurately the development of a child’s microbiome and/or its relative state of repair.
Next, they turned to mice colonized with the same collections of microbes found in the intestines of the Bangladeshi children. Gordon’s team then tinkered with the animals’ diets in search of ingredients commonly consumed by young children in Bangladesh that also appeared to encourage a healthier, more mature microbiome. They did similar studies in young pigs, whose digestive and immune systems more closely resemble humans.
The Gordon team settled on three candidate microbiome-friendly formulations. Two included chickpea flour, soy flour, peanut flour, and banana at different concentrations; one of these two also included milk powder. The third combined chickpea flour and soy flour. All three contained similar amounts of protein, fat, and calories.
The researchers then launched a randomized, controlled clinical trial with children from a year to 18 months old with moderate acute malnutrition. These young children were enrolled into one of four treatment groups, each including 14 to 17 kids. Three groups received one of the newly formulated foods. The fourth group received standard rice-and-lentil-based meals.
The children received these supplemental meals twice a day for four weeks at the International Centre for Diarrhoeal Disease Research followed by two-weeks of observation. Mothers were encouraged throughout the study to continue breastfeeding their children.
The formulation containing chickpea, soy, peanut, and banana, but no milk powder, stood out above the rest in the study. Children taking this supplement showed a dramatic shift toward a healthier state as measured by those more than 1,300 blood proteins. Their gut microbiomes also resembled those of healthy children their age.
Their new findings published in the journal Science offer the first evidence that a therapeutic food, developed to support the growth and development of a healthy microbiome, might come with added benefits for children suffering from malnutrition. Importantly, the researchers took great care to design the supplements with foods that are readily available, affordable, culturally acceptable, and palatable for young children in Bangladesh.
A month isn’t nearly long enough to see how the new foods would help children grow and recover over time. So, the researchers are now conducting a much larger study of their leading supplement in children with histories of malnutrition, to explore its longer-term health effects for them and their microbiomes. The hope is that these new foods and others adapted for use around the world soon will help many more kids grow up to be healthy adults.
References:
[1] Effects of microbiota-directed foods in gnotobiotic animals and undernourished children. Gehrig JL, Venkatesh S, Chang HW, Hibberd MC, Kung VL, Cheng J, Chen RY, Subramanian S, Cowardin CA, Meier MF, O’Donnell D, Talcott M, Spears LD, Semenkovich CF, Henrissat B, Giannone RJ, Hettich RL, Ilkayeva O, Muehlbauer M, Newgard CB, Sawyer C, Head RD, Rodionov DA, Arzamasov AA, Leyn SA, Osterman AL, Hossain MI, Islam M, Choudhury N, Sarker SA, Huq S, Mahmud I, Mostafa I, Mahfuz M, Barratt MJ, Ahmed T, Gordon JI. Science. 2019 Jul 12;365(6449).
[2] Childhood Malnutrition. World Health Organization
[3] Persistent gut microbiota immaturity in malnourished Bangladeshi children. Subramanian S, Huq S, Yatsunenko T, Haque R, Mahfuz M, Alam MA, Benezra A, DeStefano J, Meier MF, Muegge BD, Barratt MJ, VanArendonk LG, Zhang Q, Province MA, Petri WA Jr, Ahmed T, Gordon JI. Nature. 2014 Jun 19;510(7505):417-21.
[4] Gut bacteria that prevent growth impairments transmitted by microbiota from malnourished children. Blanton LV, Charbonneau MR, Salih T, Barratt MJ, Venkatesh S, Ilkaveya O, Subramanian S, Manary MJ, Trehan I, Jorgensen JM, Fan YM, Henrissat B, Leyn SA, Rodionov DA, Osterman AL, Maleta KM, Newgard CB, Ashorn P, Dewey KG, Gordon JI. Science. 2016 Feb 19;351(6275).
[5] A sparse covarying unit that describes healthy and impaired human gut microbiota development. Raman AS, Gehrig JL, Venkatesh S, Chang HW, Hibberd MC, Subramanian S, Kang G, Bessong PO, Lima AAM, Kosek MN, Petri WA Jr, Rodionov DA, Arzamasov AA, Leyn SA, Osterman AL, Huq S, Mostafa I, Islam M, Mahfuz M, Haque R, Ahmed T, Barratt MJ, Gordon JI. Science. 2019 Jul 12;365(6449).
Links:
Childhood Nutrition Facts (Centers for Disease Control and Prevention)
Gordon Lab (Washington University School of Medicine in St. Louis)
International Centre for Diarrhoeal Disease Research (Dhaka, Bangladesh)
NIH Support: National Institute of Diabetes and Digestive and Kidney Diseases; National Institute of General Medical Sciences; National Institute of Arthritis and Musculoskeletal and Skin Diseases; National Center for Advancing Translational Sciences; National Cancer Institute
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Posted In: News
Tags: bacteria, banana, Bangladesh, chickpeas, childiren, clinical trial, development, diet, food, global health, gut microbiome, immature microbiome, infants, International Centre for Diarrhoeal Disease Researc, intestine, malnutrition, metabolism, microbiome, microbiota, nutrition, peanut, poverty, soy
Expanding Our View of the Human Microbiome
Posted on by Dr. Francis Collins
 Many people still regard bacteria and other microbes just as disease-causing germs. But it’s a lot more complicated than that. In fact, it’s become increasingly clear that the healthy human body is teeming with microorganisms, many of which play essential roles in our metabolism, our immune response, and even our mental health. We are not just an organism, we are a “superorganism” made up of human cells and microbial cells—and the microbes outnumber us! Fueling this new understanding is NIH’s Human Microbiome Project (HMP), a quest begun a decade ago to explore the microbial makeup of healthy Americans.
Many people still regard bacteria and other microbes just as disease-causing germs. But it’s a lot more complicated than that. In fact, it’s become increasingly clear that the healthy human body is teeming with microorganisms, many of which play essential roles in our metabolism, our immune response, and even our mental health. We are not just an organism, we are a “superorganism” made up of human cells and microbial cells—and the microbes outnumber us! Fueling this new understanding is NIH’s Human Microbiome Project (HMP), a quest begun a decade ago to explore the microbial makeup of healthy Americans.
About 5 years ago, HMP researchers released their first round of data that provided a look at the microbes present in the mouth, gut, nose, and several other parts of the body [1]. Now, their second wave of data, just published in the journal Nature, has tripled this treasure trove of information, promising to further expand our understanding of the human microbiome and its role in health and disease [2]. For example, the new DNA data offer clues as to the functional roles those microbes play and how those can vary over time in different parts of the human body and from one person to the next.
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Protein Links Gut Microbes, Biological Clocks, and Weight Gain
Posted on by Dr. Francis Collins

Caption: Lipids (red) inside mouse intestinal cells with and without NFIL3.
Credit: Lora V. Hooper, University of Texas Southwestern Medical Center, Dallas
The American epidemic of obesity is a major public health concern, and keeping off the extra pounds is a concern for many of us. Yet it can also be a real challenge for people who may eat normally but get their days and nights mixed up, including night-shift workers and those who regularly travel overseas. Why is that?
The most obvious reason is the odd hours throw a person’s 24-hour biological clock—and metabolism—out of sync. But an NIH-funded team of researchers has new evidence in mice to suggest the answer could go deeper to include the trillions of microbes that live in our guts—and, more specifically, the way they “talk” to intestinal cells. Their studies suggest that what gut microbes “say” influences the activity of a key clock-driven protein called NFIL3, which can set intestinal cells up to absorb and store more fat from the diet while operating at hours that might run counter to our fixed biological clocks.
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Creative Minds: The Human Gut Microbiome’s Top 100 Hits
Posted on by Dr. Francis Collins
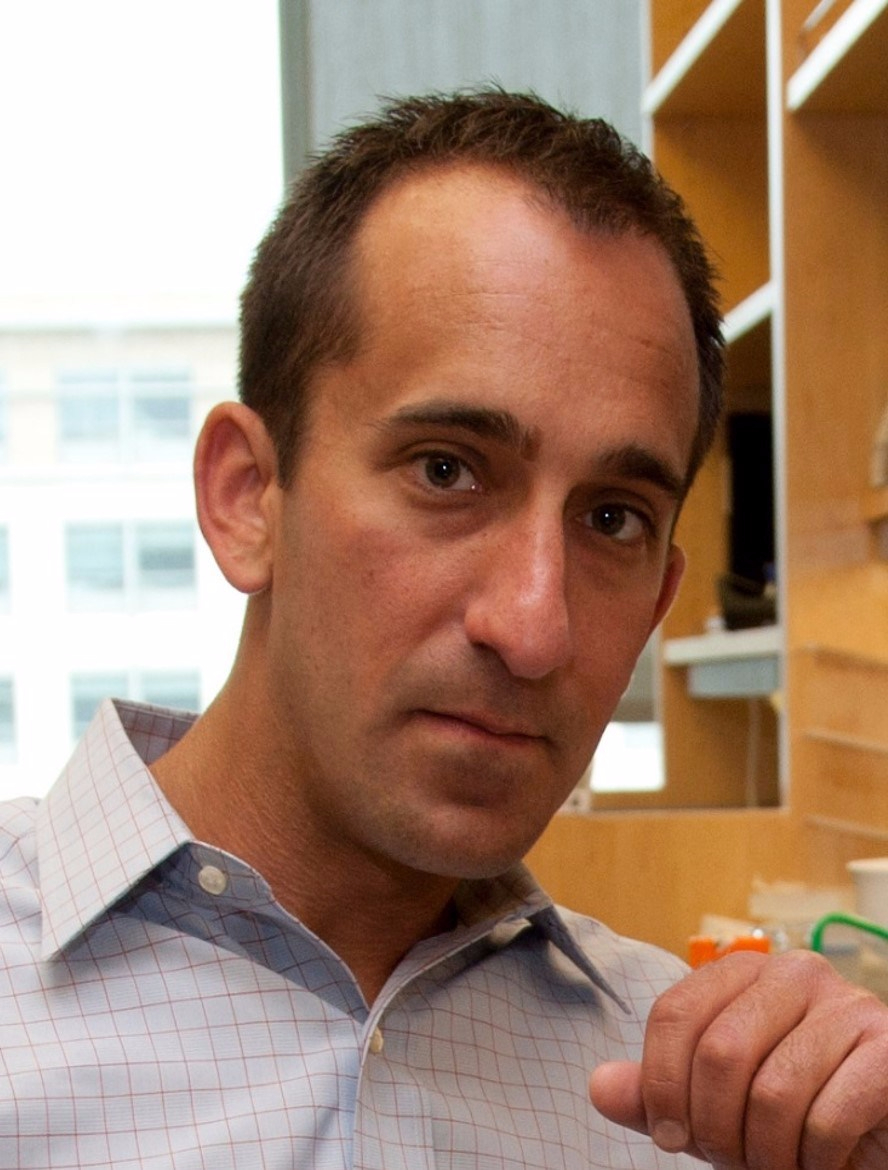
Michael Fishbach
Microbes that live in dirt often engage in their own deadly turf wars, producing a toxic mix of chemical compounds (also called “small molecules”) that can be a source of new antibiotics. When he started out in science more than a decade ago, Michael Fischbach studied these soil-dwelling microbes to look for genes involved in making these compounds.
Eventually, Fischbach, who is now at the University of California, San Francisco, came to a career-altering realization: maybe he didn’t need to dig in dirt! He hypothesized an even better way to improve human health might be found in the genes of the trillions of microorganisms that dwell in and on our bodies, known collectively as the human microbiome.
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Tags: 2016 NIH Director’s Pioneer Award, analytical chemistry, antibiotics, bacteria, biochemistry, biofilm, digestion, gastrointestinal disease, gastrointestinal tract, genetic engineering, genetics, GI tract, gut, gut bacteria, gut microbiome, heart disease, microbes, microbiome, microbiota, microorganisms, obesity, probiotics, small molecules, synthetic gut community
