infection
3D Animation Captures Viral Infection in Action
Posted on by Lawrence Tabak, D.D.S., Ph.D.
With the summer holiday season now in full swing, the blog will also swing into its annual August series. For most of the month, I will share with you just a small sampling of the colorful videos and snapshots of life captured in a select few of the hundreds of NIH-supported research labs around the country.
To get us started, let’s turn to the study of viruses. Researchers now can generate vast amounts of data relatively quickly on a virus of interest. But data are often displayed as numbers or two-dimensional digital images on a computer screen. For most virologists, it’s extremely helpful to see a virus and its data streaming in three dimensions. To do so, they turn to a technological tool that we all know so well: animation.
This research animation features the chikungunya virus, a sometimes debilitating, mosquito-borne pathogen transmitted mainly in developing countries in Africa, Asia and the Americas. The animation illustrates large amounts of research data to show how the chikungunya virus infects our cells and uses its specialized machinery to release its genetic material into the cell and seed future infections. Let’s take a look.
In the opening seconds, you see how receptor binding glycoproteins (light blue), which are proteins with a carbohydrate attached on the viral surface, dock with protein receptors (yellow) on a host cell. At five seconds, the virus is drawn inside the cell. The change in the color of the chikungunya particle shows that it’s coated in a vesicle, which helps the virus make its way unhindered through the cytoplasm.
At 10 seconds, the virus then enters an endosome, ubiquitous bubble-like compartments that transport material from outside the cell into the cytosol, the fluid part of the cytoplasm. Once inside the endosome, the acidic environment makes other glycoproteins (red, blue, yellow) on the viral surface change shape and become more flexible and dynamic. These glycoproteins serve as machinery that enables them to reach out and grab onto the surrounding endosome membrane, which ultimately will be fused with the virus’s own membrane.
As more of those fusion glycoproteins grab on, fold back on themselves, and form into hairpin-like shapes, they pull the membranes together. The animation illustrates not only the changes in protein organization, but the resulting effects on the integrity of the membrane structures as this dynamic process proceeds. At 53 seconds, the viral protein shell, or capsid (green), which contains the virus’ genetic instructions, is released back out into the cell where it will ultimately go on to make more virus.
This remarkable animation comes from Margot Riggi and Janet Iwasa, experts in visualizing biology at the University of Utah’s Animation Lab, Salt Lake City. Their data source was researcher Kelly Lee, University of Washington, Seattle, who collaborated closely with Riggi and Iwasa on this project. The final product was considered so outstanding that it took the top prize for short videos in the 2022 BioArt Awards competition, sponsored by the Federation of American Societies for Experimental Biology (FASEB).
The Lee lab uses various research methods to understand the specific shape-shifting changes that chikungunya and other viruses perform as they invade and infect cells. One of the lab’s key visual tools is cryo-electron microscopy (Cryo-EM), specifically cryo-electron tomography (cryo-ET). Cryto-ET enables complex 3D structures, including the intermediate state of biological reactions, to be captured and imaged in remarkably fine detail.
In a study in the journal Nature Communications [1] last year, Lee’s team used cryo-ET to reveal how the chikungunya virus invades and delivers its genetic cargo into human cells to initiate a new infection. While Lee’s cryo-ET data revealed stages of the virus entry process and fine structural details of changes to the virus as it enters a cell and starts an infection, it still represented a series of snapshots with missing steps in between. So, Lee’s lab teamed up with The Animation Lab to help beautifully fill in the gaps.
Visualizing chikungunya and similar viruses in action not only makes for informative animations, it helps researchers discover better potential targets to intervene in this process. This basic research continues to make progress, and so do ongoing efforts to develop a chikungunya vaccine [2] and specific treatments that would help give millions of people relief from the aches, pains, and rashes associated with this still-untreatable infection.
References:
[1] Visualization of conformational changes and membrane remodeling leading to genome delivery by viral class-II fusion machinery. Mangala Prasad V, Blijleven JS, Smit JM, Lee KK. Nat Commun. 2022 Aug 15;13(1):4772. doi: 10.1038/s41467-022-32431-9. PMID: 35970990; PMCID: PMC9378758.
[2] Experimental chikungunya vaccine is safe and well-tolerated in early trial, National Institute of Allergy and Infectious Diseases news release, April 27, 2020.
Links:
Chikungunya Virus (Centers for Disease Control and Prevention, Atlanta)
Global Arbovirus Initiative (World Health Organization, Geneva, Switzerland)
The Animation Lab (University of Utah, Salt Lake City)
Video: Janet Iwasa (TED Speaker)
Lee Lab (University of Washington, Seattle)
BioArt Awards (Federation of American Societies for Experimental Biology, Rockville, MD)
NIH Support: National Institute of General Medical Sciences; National Institute of Allergy and Infectious Diseases
How Mucus Tames Microbes
Posted on by Dr. Francis Collins
Most of us think of mucus as little more than slimy and somewhat yucky stuff that’s easily ignored until you come down with a cold like the one I just had. But, when it comes to our health, there’s much more to mucus than you might think.
Mucus covers the moist surfaces of the human body, including the eyes, nostrils, lungs, and gastrointestinal tract. In fact, the average person makes more than a liter of mucus each day! It houses trillions of microbes and serves as a first line of defense against the subset of those microorganisms that cause infections. For these reasons, NIH-funded researchers, led by Katharina Ribbeck, Massachusetts Institute of Technology, Cambridge, are out to gain a greater understanding of the biology of healthy mucus—and then possibly use that knowledge to develop new therapeutics.
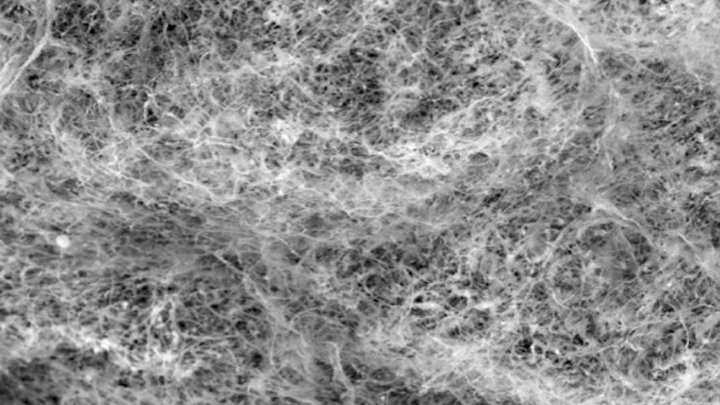
Ribbeck’s team used a scanning electron microscope to take the image of mucus you see above. You’ll notice right away that mucus doesn’t look like simple slime at all. In fact, if you could zoom into this complex web, you’d discover it’s made up of mucin proteins and glycans, which are sugar molecules that resemble bottle brushes.
Ribbeck and her colleagues recently discovered that the glycans in healthy mucus play a long-overlooked role in “taming” bacteria that might make us ill [1]. This work builds on their previous findings that mucus interferes with bacterial behavior, preventing these bugs from attaching to surfaces and communicating with each other [2].
In their new study, published in Nature Microbiology, Ribbeck, lead author Kelsey Wheeler, and their colleagues studied mucus and its interactions with Pseudomonas aeruginosa. This bacterium is a common cause of serious lung infections in people with cystic fibrosis or compromised immune systems.
The researchers found that in the presence of glycans, P. aeruginosa was rendered less harmful and infectious. The bacteria also produced fewer toxins. The findings show that it isn’t just that microbes get trapped in a tangled web within mucus, but rather that glycans have a special ability to moderate the bugs’ behavior. The researchers also have evidence of similar interactions between mucus and other microorganisms, such as those responsible for yeast infections.
The new study highlights an intriguing strategy to tame, rather than kill, bacteria to manage infections. In fact, Ribbeck views mucus and its glycans as a therapeutic gold mine. She hopes to apply what she’s learned to develop artificial mucus as an anti-microbial therapeutic for use inside and outside the body. Not bad for a substance that you might have thought was nothing more than slimy stuff.
References:
[1] Mucin glycans attenuate the virulence of Pseudomonas aeruginosa in infection. Wheeler KM, Cárcamo-Oyarce G, Turner BS, Dellos-Nolan S, Co JY, Lehoux S, Cummings RD, Wozniak DJ, Ribbeck K. Nat Microbiol. 2019 Oct 14.
[2] Mucins trigger dispersal of Pseudomonas aeruginosa biofilms. Co JY, Cárcamo-Oyarce, Billings N, Wheeler KM, Grindy SC, Holten-Andersen N, Ribbeck K. NPJ Biofilms Microbiomes. 2018 Oct 10;4:23.
Links:
Cystic Fibrosis (National Heart, Lung, and Blood Institute/NIH)
Video: Chemistry in Action—Katharina Ribbeck (YouTube)
Katharina Ribbeck (Massachusetts Institute of Technology, Cambridge)
NIH Support: National Institute of Biomedical Imaging and Bioengineering; National Institute of Environmental Health Sciences; National Institute of General Medical Sciences; National Institute of Allergy and Infectious Diseases
How Measles Leave the Body Prone to Future Infections
Posted on by Dr. Francis Collins

As a kid who was home-schooled on a Virginia farm in the 1950s, I wasn’t around other kids very much, and so didn’t get exposed to measles. And there was no vaccine yet. Later on as a medical resident, I didn’t recognize that I wasn’t immune. So when I was hospitalized with a severe febrile illness at age 29, it took a while to figure out the diagnosis. Yes, it was measles. I have never been that sick before or since. I was lucky not to have long-term consequences, and now I’m learning that there may be even more to consider.
With the big push to get kids vaccinated, you’ve probably heard about some of the very serious complications of measles: hearing-threatening ear infections, bronchitis, laryngitis, and even life-threatening forms of pneumonia and encephalitis. But now comes word of yet another way in which the measles can be devastating—one that may also have long-term consequences for a person’s health.
In a new study in the journal Science, a research team, partly funded by NIH, found that the measles virus not only can make children deathly ill, it can cause their immune systems to forget how to ward off other common infections [1]. The virus does this by wiping out up to nearly three-quarters of the protective antibodies that a child’s body has formed in response to past microbial invaders and vaccinations. This immune “amnesia” can leave a child more vulnerable to re-contracting infections, such as influenza or respiratory syncytial virus (RSV), that they may have been protected against before they came down with measles.
The finding comes as yet another reason to feel immensely grateful that, thanks to our highly effective vaccination programs, most people born in the U.S. from the 1960s onward should never have to experience the measles.
There had been hints that the measles virus might somehow suppress a person’s immune system. Epidemiological evidence also had suggested that measles infections might lead to increased susceptibility to infection for years afterwards [2]. Scientists had even suspected this might be explained by a kind of immune amnesia. The trouble was that there wasn’t any direct proof that such a phenomenon actually existed.
In the new work, the researchers, led by Michael Mina, Tomasz Kula, and Stephen Elledge, Howard Hughes Medical Institute and Brigham and Women’s Hospital, Boston, took advantage of a tool developed a few years ago in the Elledge lab called VirScan [3]. VirScan detects antibodies in blood samples acquired as a result of a person’s past encounters with hundreds of viruses, bacteria, or vaccines, providing a comprehensive snapshot of acquired immunity at a particular moment in time.
To look for evidence of immune amnesia following the measles, the research team needed blood samples gathered from people both before and after infection. These types of samples are currently hard to come by in the U.S. thanks to the success of vaccines. By partnering with Rik de Swart, Erasmus University Medical Center, Rotterdam, Netherlands, they found the samples that they needed.
During a recent measles outbreak in the Netherlands, de Swart had gathered blood samples from children living in communities with low vaccination rates. Elledge’s group used VirScan with 77 unvaccinated kids to measure antibodies in samples collected before and about two months after their measles infections.
That included 34 children who had mild infections and 43 who had severe measles. The researchers also examined blood samples from five children who remained uninfected and 110 kids who hadn’t been exposed to the measles virus.
The VirScan data showed that the infected kids, not surprisingly, produced antibodies to the measles virus. But their other antibodies dropped and seemed to be disappearing. In fact, depending on the severity of measles infection, the kids showed on average a loss of around 40 percent of their antibody memory, with greater losses in children with severe cases of the measles. In at least one case, the loss reached a whopping 73 percent.
This all resonates with me. I do recall that after my bout with the measles, I seemed to be coming down with a lot of respiratory infections. I attributed that to the lifestyle of a medical resident—being around lots of sick patients and not getting much sleep. But maybe it was more than that.
The researchers suggest that the loss of immune memory may stem from the measles virus destroying some of the long-lived cells in bone marrow. These cells remember past infections and, based on that immunological memory, churn out needed antibodies to thwart reinvading viruses.
Interestingly, after a measles infection, the children’s immune systems still responded to new infections and could form new immune memories. But it appears the measles caused long term, possibly permanent, losses of a significant portion of previously acquired immunities. This loss of immune memory put the children at a distinct disadvantage should those old bugs circulate again.
It’s important to note that, unlike measles infection, the MMR (measles, mumps, rubella) vaccine does NOT compromise previously acquired immunity. So, these findings come as yet another reminder of the public value of measles vaccination.
Prior to 1963, when the measles vaccine was developed, 3 to 4 million Americans got the measles each year. As more people were vaccinated, the incidence of measles plummeted. By the year 2000, the disease was declared eliminated from the U.S.
Unfortunately, measles has made a come back, fueled by vaccine refusals. In October, the Centers for Disease Control and Prevention (CDC) reported an estimated 1,250 measles cases in the United States so far in 2019, surpassing the total number of cases reported annually in each of the past 25 years [4].
Around the world, measles continues to infect 7 million people each year, leading to an estimated 120,000 deaths. Based on the new findings, Elledge’s team now suspects the actual toll of the measles may be five times greater, due to the effects of immune amnesia.
The good news is those numbers can be reduced if more people get the vaccine, which has been shown repeatedly in many large and rigorous studies to be safe and effective. The CDC recommends that children should receive their first dose by 12 to 15 months of age and a second dose between the ages of 4 and 6. Older people who’ve been vaccinated or have had the measles previously should consider being re-vaccinated, especially if they live in places with low vaccination rates or will be traveling to countries where measles are endemic.
References:
[1] Measles virus infection diminishes preexisting antibodies that offer protection from other pathogens. Mina MJ, Kula T, Leng Y, Li M, de Vries RD, Knip M, Siljander H, Rewers M, Choy DF, Wilson MS, Larman HB, Nelson AN, Griffin DE, de Swart RL, Elledge SJ. et al. Science. 2019 Nov 1; 366 (6465): 599-606.
[2] Long-term measles-induced immunomodulation increases overall childhood infectious disease mortality. Mina MJ, Metcalf CJE, De Swart RL, Osterhaus ADME, Grenfell BT. Science. 2015 May 8; 348(6235).
[3] Viral immunology. Comprehensive serological profiling of human populations using a synthetic human virome. Xu GJ, Kula T, Xu Q, Li MZ, Vernon SD, Ndung’u T, Ruxrungtham K, Sanchez J, Brander C, Chung RT, O’Connor KC, Walker B, Larman HB, Elledge SJ. Science. 2015 Jun 5;348(6239):aaa0698.
[4] Measles cases and outbreaks. Centers for Disease Control and Prevention. Oct. 11, 2019.
Links:
Measles (MedlinePlus Medical Encyclopedia/National Library of Medicine/NIH)
Measles History (Centers for Disease Control and Prevention)
Vaccines (National Institute of Allergy and Infectious Diseases/NIAID)
Vaccines Protect Your Community (Vaccines.gov)
Elledge Lab (Harvard Medical School, Boston)
NIH Support: National Institute of Allergy and Infectious Diseases; National Institute of Diabetes and Digestive and Kidney Diseases
Some ‘Hospital-Acquired’ Infections Traced to Patient’s Own Microbiome
Posted on by Dr. Francis Collins
Caption: New computational tool determines whether a gut microbe is the source of a hospital-acquired bloodstream infection
Credit: Fiona Tamburini, Stanford University, Palo Alto, CA
While being cared for in the hospital, a disturbingly large number of people develop potentially life-threatening bloodstream infections. It’s been thought that most of the blame lies with microbes lurking on medical equipment, health-care professionals, or other patients and visitors. And certainly that is often true. But now an NIH-funded team has discovered that a significant fraction of these “hospital-acquired” infections may actually stem from a quite different source: the patient’s own body.
In a study of 30 bone-marrow transplant patients suffering from bloodstream infections, researchers used a newly developed computational tool called StrainSifter to match microbial DNA from close to one-third of the infections to bugs already living in the patients’ large intestines [1]. In contrast, the researchers found little DNA evidence to support the notion that such microbes were being passed around among patients.
Portable System Uses Light to Diagnose Bacterial Infections Faster
Posted on by Dr. Francis Collins

Caption: PAD system. Left, four optical testing cubes (blue and white) stacked on the electronic base station (white with initials); right, a smartphone with a special app to receive test results transmitted by the electronic base station.
Credit: Park et al. Sci. Adv. 2016
Every year, hundreds of thousands of Americans acquire potentially life-threatening bacterial infections while in the hospital, nursing home, or other health-care settings [1]. Such infections can be caused by a variety of bacteria, which may respond quite differently to different antibiotics. To match a patient with the most appropriate antibiotic therapy, it’s crucial to determine as quickly as possible what type of bacteria is causing his or her infection. In an effort to improve that process, an NIH-funded team is working to develop a point-of-care system and smartphone app aimed at diagnosing bacterial infections in a faster, more cost-effective manner.
The portable new system, described recently in the journal Science Advances, uses a novel light-based method for detecting telltale genetic sequences from bacteria in bodily fluids, such as blood, urine, or drainage from a skin abscess. Testing takes place within small, optical cubes that, when placed on an electronic base station, deliver test results within a couple of hours via a simple readout sent directly to a smartphone [2]. When the system was tested on clinical samples from a small number of hospitalized patients, researchers found that not only did it diagnose bacterial infections about as accurately and more swiftly than current methods, but it was also cheaper. This new system can potentially also be used to test for the presence of antibiotic-resistant bacteria and contamination of medical devices.
MRSA in a New Light
Posted on by Dr. Francis Collins

At first glance, this image looks like something pulled from the files of NASA, not NIH. But, no, you are not looking at alien orbs on the rocky surface of some distant planet! This is a colorized scanning electron micrograph of a white blood cell eating an antibiotic resistant strain of Staphylococcus aureus bacteria, commonly known as MRSA.
MRSA stands for methicillin-resistant Staphylococcus aureus, and it’s one nasty bug. You’ve probably heard about the dangers of MRSA infections, but what’s the easiest way to prevent one? Just like with the flu, you should wash your hands – frequently! Personal hygiene is key. And while MRSA infections are more common in people with weakened immune systems, other folks, such as athletes who share towels, are also vulnerable. To learn more about MRSA and how to protect yourself and your loved ones from this increasingly common health risk, go to http://www.nlm.nih.gov/medlineplus/ency/article/007261.htm.
