family studies
COVID-19 Vaccines Protect the Family, Too
Posted on by Dr. Francis Collins

Any of the available COVID-19 vaccines offer remarkable personal protection against the coronavirus SARS-CoV-2. So, it also stands to reason that folks who are vaccinated will reduce the risk of spreading the virus to family members within their households. That protection is particularly important when not all family members can be immunized—as when there are children under age 12 or adults with immunosuppression in the home. But just how much can vaccines help to protect families from COVID-19 when only some, not all, in the household have immunity?
A Swedish study, published recently in the journal JAMA Internal Medicine, offers some of the first hard figures on this topic, and the findings are quite encouraging [1]. The data show that people without any immunity against COVID-19 were at considerably lower risk of infection and hospitalization when other members of their family had immunity, either from a natural infection or vaccination. In fact, the protective effect on family members went up as the number of immune family members increased.
The findings come from a team led by Peter Nordström, Umeå University, Sweden. Like in the United States, vaccinations in Sweden initially were prioritized for high-risk groups and people with certain preexisting conditions. As a result, Swedish families have functioned, often in close contact, as a mix of immune and susceptible individuals over the course of the pandemic.
To explore these family dynamics in greater detail, the researchers relied on nationwide registries to identify all Swedes who had immunity to SARS-COV-2 from either a confirmed infection or vaccination by May 26, 2021. The researchers identified more than 5 million individuals who’d been either diagnosed with COVID-19 or vaccinated and then matched them to a control group without immunity. They also limited the analysis to individuals in families with two to five members of mixed immune status.
This left them with about 1.8 million people from more than 800,000 families. The situation in Sweden is also a little unique from most Western nations. Somewhat controversially, the Swedish government didn’t order a mandatory citizen quarantine to slow the spread of the virus.
The researchers found in the data a rising protective effect for those in the household without immunity as the number of immune family members increased. Families with one immune family member had a 45 to 61 percent lower risk of a COVID-19 infection in the home than those who had none. Those with two immune family members enjoyed more protection, with a 75 to 86 percent reduction in risk of COVID-19. For those with three or four immune family members, the protection went up to more than 90 percent, topping out at 97 percent protection. The results were similar when the researchers limited the analysis to COVID-19 illnesses serious enough to warrant a hospital stay.
The findings confirm that vaccination is incredibly important not only for individual protection, but also for reducing transmission, especially within families and those with whom we’re in close physical contact. It’s also important to note that the findings apply to the original SARS-CoV-2 variant, which was dominant when the study was conducted. But we know that the vaccines offer good protection against Delta and other variants of concern.
These results show quite clearly that vaccines offer protection for individuals who lack immunity, with important implications for finally ending this pandemic. This doesn’t change the fact that all those who can and still need to get fully vaccinated should do so as soon as possible. If you are eligible for a booster shot, that’s something to consider, too. But, if for whatever reason you haven’t gotten vaccinated just yet, perhaps these new findings will encourage you to do it now for the sake of those other people you care about. This is a chance to love your family—and love your neighbor.
Reference:
[1] Association between risk of COVID-19 infection in nonimmune individuals and COVID-19 immunity in their family members. Nordström P, Ballin M, Nordström A. JAMA Intern Med. 2021 Oct 11.
Links:
COVID-19 Research (NIH)
Peter Nordström (Umeå University, Sweden)
Crowdsourcing 600 Years of Human History
Posted on by Dr. Francis Collins
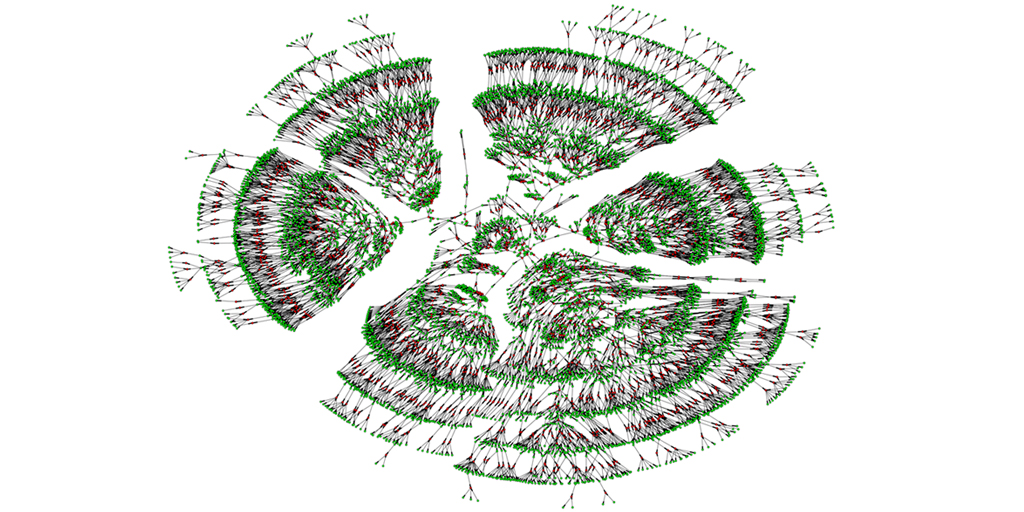
Caption: A 6,000-person family tree, showing individuals spanning seven generations (green) and their marital links (red).
Credit: Columbia University, New York City
You may have worked on constructing your family tree, perhaps listing your ancestry back to your great-grandparents. Or with so many public records now available online, you may have even uncovered enough information to discover some unexpected long-lost relatives. Or maybe you’ve even submitted a DNA sample to one of the commercial sources to see what you could learn about your ancestry. But just how big can a family tree grow using today’s genealogical tools?
A recent paper offers a truly eye-opening answer. With permission to download the publicly available, online profiles of 86 million genealogy hobbyists, most of European descent, the researchers assembled more than 5 million family trees. The largest totaled more than 13 million people! By merging each tree from the crowd-sourced and public data, including the relatively modest 6,000-person seedling shown above, the researchers were able to go back 11 generations on average to the 15th century and the days of Christopher Columbus. Doubly exciting, these large datasets offer a powerful new resource to study human health, having already provided some novel insights into our family structures, genes, and longevity.
Creative Minds: Opening a Window on Alzheimer’s Before It Strikes
Posted on by Dr. Francis Collins
While attending college in her native Colombia, Yakeel T. Quiroz joined the Grupo de Neurociencias de Antioquia. This dedicated group of Colombian researchers, healthcare workers, and students has worked for many years with a large extended family in the northwestern district of Antioquia that is truly unique.
About half of the more than 5,000 family members inherit a gene mutation that predisposes them to what is known locally as “la bobera,” or “the foolishness,” a devastating form of early-onset Alzheimer’s disease. Those born with the mutation are cognitively healthy through their 20s, become forgetful in their 30s, and descend into full-blown Alzheimer’s disease by their mid-to-late 40s. Making matters worse, multiple family members sometimes are in different stages of dementia at the same time, including the caregiver attempting to hold the household together.
Quiroz, now a researcher at Massachusetts General Hospital, Boston, vowed never to forget these families. She hasn’t, working hard to understand early-onset Alzheimer’s disease and helping to establish the Forget Me Not Initiative to raise money for affected families. With an NIH Director’s Early Independence Award, Quiroz also recently launched her own lab to pursue an even broader scientific opportunity: discover subtle pre-symptomatic changes in the brain years before they give rise to detectable Alzheimer’s. What she learns will have application not only to detect and possibly treat early-onset Alzheimer’s in Colombia but also to understand the late-onset forms of the dementia that affect an estimated 35.6 million people worldwide.

