wearable biosensors
Giving Thanks for Biomedical Research
Posted on by Dr. Francis Collins
This Thanksgiving, Americans have an abundance of reasons to be grateful—loving family and good food often come to mind. Here’s one more to add to the list: exciting progress in biomedical research. To check out some of that progress, I encourage you to watch this short video, produced by NIH’s National Institute of Biomedical Imaging and Engineering (NIBIB), that showcases a few cool gadgets and devices now under development.
Among the technological innovations is a wearable ultrasound patch for monitoring blood pressure [1]. The patch was developed by a research team led by Sheng Xu and Chonghe Wang, University of California San Diego, La Jolla. When this small patch is worn on the neck, it measures blood pressure in the central arteries and veins by emitting continuous ultrasound waves.
Other great technologies featured in the video include:
• Laser-Powered Glucose Meter. Peter So and Jeon Woong Kang, researchers at Massachusetts Institute of Technology (MIT), Cambridge, and their collaborators at MIT and University of Missouri, Columbia have developed a laser-powered device that measures glucose through the skin [2]. They report that this device potentially could provide accurate, continuous glucose monitoring for people with diabetes without the painful finger pricks.
• 15-Second Breast Scanner. Lihong Wang, a researcher at California Institute of Technology, Pasadena, and colleagues have combined laser light and sound waves to create a rapid, noninvasive, painless breast scan. It can be performed while a woman rests comfortably on a table without the radiation or compression of a standard mammogram [3].
• White Blood Cell Counter. Carlos Castro-Gonzalez, then a postdoc at Massachusetts Institute of Technology, Cambridge, and colleagues developed a portable, non-invasive home monitor to count white blood cells as they pass through capillaries inside a finger [4]. The test, which takes about 1 minute, can be carried out at home, and will help those undergoing chemotherapy to determine whether their white cell count has dropped too low for the next dose, avoiding risk for treatment-compromising infections.
• Neural-Enabled Prosthetic Hand (NEPH). Ranu Jung, a researcher at Florida International University, Miami, and colleagues have developed a prosthetic hand that restores a sense of touch, grip, and finger control for amputees [5]. NEPH is a fully implantable, wirelessly controlled system that directly stimulates nerves. More than two years ago, the FDA approved a first-in-human trial of the NEPH system.
If you want to check out more taxpayer-supported innovations, take a look at NIBIB’s two previous videos from 2013 and 2018 As always, let me offer thanks to you from the NIH family—and from all Americans who care about the future of their health—for your continued support. Happy Thanksgiving!
References:
[1] Monitoring of the central blood pressure waveform via a conformal ultrasonic device. Wang C, Li X, Hu H, Zhang, L, Huang Z, Lin M, Zhang Z, Yun Z, Huang B, Gong H, Bhaskaran S, Gu Y, Makihata M, Guo Y, Lei Y, Chen Y, Wang C, Li Y, Zhang T, Chen Z, Pisano AP, Zhang L, Zhou Q, Xu S. Nature Biomedical Engineering. September 2018, 687-695.
[2] Evaluation of accuracy dependence of Raman spectroscopic models on the ratio of calibration and validation points for non-invasive glucose sensing. Singh SP, Mukherjee S, Galindo LH, So PTC, Dasari RR, Khan UZ, Kannan R, Upendran A, Kang JW. Anal Bioanal Chem. 2018 Oct;410(25):6469-6475.
[3] Single-breath-hold photoacoustic computed tomography of the breast. Lin L, Hu P, Shi J, Appleton CM, Maslov K, Li L, Zhang R, Wang LV. Nat Commun. 2018 Jun 15;9(1):2352.
[4] Non-invasive detection of severe neutropenia in chemotherapy patients by optical imaging of nailfold microcirculation. Bourquard A, Pablo-Trinidad A, Butterworth I, Sánchez-Ferro Á, Cerrato C, Humala K, Fabra Urdiola M, Del Rio C, Valles B, Tucker-Schwartz JM, Lee ES, Vakoc BJ9, Padera TP, Ledesma-Carbayo MJ, Chen YB, Hochberg EP, Gray ML, Castro-González C. Sci Rep. 2018 Mar 28;8(1):5301.
[5] Enhancing Sensorimotor Integration Using a Neural Enabled Prosthetic Hand System
Links:
Sheng Xu Lab (University of California San Diego, La Jolla)
So Lab (Massachusetts Institute of Technology, Cambridge)
Lihong Wang (California Institute of Technology, Pasadena)
Video: Lihong Wang: Better Cancer Screenings
Carlos Castro-Gonzalez (Madrid-MIT M + Visión Consortium, Cambridge, MA)
Video: Carlos Castro-Gonzalez (YouTube)
Ranu Jung (Florida International University, Miami)
Video: New Prosthetic System Restores Sense of Touch (Florida International)
NIH Support: National Institute of Biomedical Imaging and Bioengineering; National Institute of Neurological Diseases and Stroke; National Heart, Lung, and Blood Institute; National Cancer Institute; Common Fund
Wearable Ultrasound Patch Monitors Blood Pressure
Posted on by Dr. Francis Collins
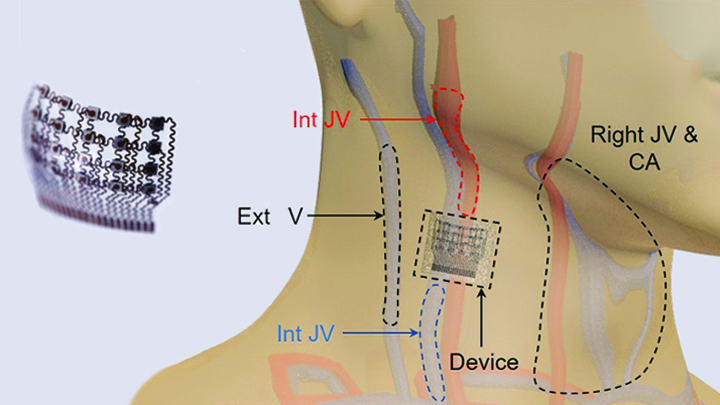
Caption: Worn on the neck, the device records central blood pressure in the carotid artery (CA), internal jugular vein (Int JV) and external jugular vein (Ext JV).
Credit: Adapted from Wang et al, Nature Biomedical Engineering
There’s lots of excitement out there about wearable devices quietly keeping tabs on our health—morning, noon, and night. Most wearables monitor biological signals detectable right at the surface of the skin. But, the sensing capabilities of the “skin” patch featured here go far deeper than that.
As described recently in Nature Biomedical Engineering, when this small patch is worn on the neck, it measures blood pressure way down in the central arteries and veins more than an inch beneath the skin [1]. The patch works by emitting continuous ultrasound waves that monitor subtle, real-time changes in the shape and size of pulsing blood vessels, which indicate rises or drops in pressure.
Building a Smarter Bandage
Posted on by Dr. Francis Collins

Credit: Tufts University, Medford, MA
Smartphones, smartwatches, and smart electrocardiograms. How about a smart bandage?
This image features a prototype of a smart bandage equipped with temperature and pH sensors (lower right) printed directly onto the surface of a thin, flexible medical tape. You also see the “brains” of the operation: a microprocessor (upper left). When the sensors prompt the microprocessor, it heats up a hydrogel heating element in the bandage, releasing drugs and/or other healing substances on demand. It can also wirelessly transmit messages directly to a smartphone to keep patients and doctors updated.
While the smart bandage might help mend everyday cuts and scrapes, it was designed with the intent of helping people with hard-to-heal chronic wounds, such as leg and foot ulcers. Chronic wounds affect millions of Americans, including many seniors [1]. Such wounds are often treated at home and, if managed incorrectly, can lead to infections and potentially serious health problems.
Got a Great Research Idea? “All of Us” Wants to Hear It!
Posted on by Dr. Francis Collins
 One of the boldest undertakings that NIH has ever attempted, the All of Us Research Program has been hard at work in a “beta” testing phase, and is now busy gearing up for full recruitment in the spring. This historic effort will enroll 1 million or more people in the United States to share information about their health, habits, and what it’s like where they live. This information will be part of a resource that scientists can use to accelerate research and improve health. How? By taking into account individual differences in lifestyle, environment, and biology, researchers will uncover paths toward realizing the full potential of precision medicine.
One of the boldest undertakings that NIH has ever attempted, the All of Us Research Program has been hard at work in a “beta” testing phase, and is now busy gearing up for full recruitment in the spring. This historic effort will enroll 1 million or more people in the United States to share information about their health, habits, and what it’s like where they live. This information will be part of a resource that scientists can use to accelerate research and improve health. How? By taking into account individual differences in lifestyle, environment, and biology, researchers will uncover paths toward realizing the full potential of precision medicine.
Before embarking on this adventure, All of Us is reaching out to prospective researchers, community organizations, and citizen scientists—including people just like you—to get their input. Imagine that the project has already enrolled 1 million participants from all over the country and from diverse backgrounds. Imagine that they have all agreed to make available their electronic health records, to put on wearable sensors that can track body physiology and environmental exposures, and to provide blood samples for lab testing, including DNA analysis. Is there a particular research question that you think All of Us could help answer? Possible topics include risks of disease, factors that promote wellness, and research on human behavior, prevention, exercise, genetics, environmental health effects, health disparities, and more. To submit an idea, just go to this special All of Us web page.
Built for the Future. Study Shows Wearable Devices Can Help Detect Illness Early
Posted on by Dr. Francis Collins

Caption: Stanford University’s Michael Snyder displays some of his wearable devices.
Credit: Steve Fisch/Stanford School of Medicine
Millions of Americans now head out the door each day wearing devices that count their steps, check their heart rates, and help them stay fit in general. But with further research, these “wearables” could also play an important role in the early detection of serious medical conditions. In partnership with health-care professionals, people may well use the next generation of wearables to monitor vital signs, blood oxygen levels, and a wide variety of other measures of personal health, allowing them to see in real time when something isn’t normal and, if unusual enough, to have it checked out right away.
In the latest issue of the journal PLoS Biology [1], an NIH-supported study offers an exciting glimpse of this future. Wearing a commercially available smartwatch over many months, more than 40 adults produced a continuous daily stream of accurate personal health data that researchers could access and monitor. When combined with standard laboratory blood tests, these data—totaling more than 250,000 bodily measurements a day per person—can detect early infections through changes in heart rate.
