Structural Biology Points Way to Coronavirus Vaccine
Posted on by Dr. Francis Collins
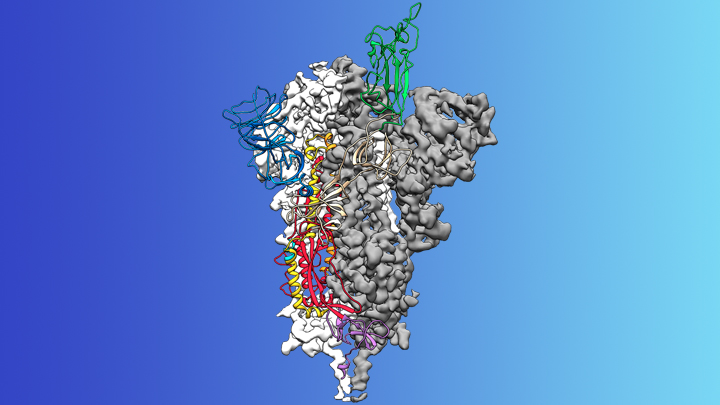
Credit: McLellan Lab, University of Texas at Austin
The recent COVID-19 outbreak of a novel type of coronavirus that began in China has prompted a massive global effort to contain and slow its spread. Despite those efforts, over the last month the virus has begun circulating outside of China in multiple countries and territories.
Cases have now appeared in the United States involving some affected individuals who haven’t traveled recently outside the country. They also have had no known contact with others who have recently arrived from China or other countries where the virus is spreading. The NIH and other U.S. public health agencies stand on high alert and have mobilized needed resources to help not only in its containment, but in the development of life-saving interventions.
On the treatment and prevention front, some encouraging news was recently reported. In record time, an NIH-funded team of researchers has created the first atomic-scale map of a promising protein target for vaccine development [1]. This is the so-called spike protein on the new coronavirus that causes COVID-19. As shown above, a portion of this spiky surface appendage (green) allows the virus to bind a receptor on human cells, causing other portions of the spike to fuse the viral and human cell membranes. This process is needed for the virus to gain entry into cells and infect them.
Preclinical studies in mice of a candidate vaccine based on this spike protein are already underway at NIH’s Vaccine Research Center (VRC), part of the National Institute of Allergy and Infectious Diseases (NIAID). An early-stage phase I clinical trial of this vaccine in people is expected to begin within weeks. But there will be many more steps after that to test safety and efficacy, and then to scale up to produce millions of doses. Even though this timetable will potentially break all previous speed records, a safe and effective vaccine will take at least another year to be ready for widespread deployment.
Coronaviruses are a large family of viruses, including some that cause “the common cold” in healthy humans. In fact, these viruses are found throughout the world and account for up to 30 percent of upper respiratory tract infections in adults.
This outbreak of COVID-19 marks the third time in recent years that a coronavirus has emerged to cause severe disease and death in some people. Earlier coronavirus outbreaks included SARS (severe acute respiratory syndrome), which emerged in late 2002 and disappeared two years later, and MERS (Middle East respiratory syndrome), which emerged in 2012 and continues to affect people in small numbers.
Soon after COVID-19 emerged, the new coronavirus, which is closely related to SARS, was recognized as its cause. NIH-funded researchers including Jason McLellan, an alumnus of the VRC and now at The University of Texas at Austin, were ready. They’d been studying coronaviruses in collaboration with NIAID investigators for years, with special attention to the spike proteins.
Just two weeks after Chinese scientists reported the first genome sequence of the virus [2], McLellan and his colleagues designed and produced samples of its spike protein. Importantly, his team had earlier developed a method to lock coronavirus spike proteins into a shape that makes them both easier to analyze structurally via the high-resolution imaging tool cryo-electron microscopy and to use in vaccine development efforts.
After locking the spike protein in the shape it takes before fusing with a human cell to infect it, the researchers reconstructed its atomic-scale 3D structural map in just 12 days. Their results, published in Science, confirm that the spike protein on the virus that causes COVID-19 is quite similar to that of its close relative, the SARS virus. It also appears to bind human cells more tightly than the SARS virus, which may help to explain why the new coronavirus appears to spread more easily from person to person, mainly by respiratory transmission.
McLellan’s team and his NIAID VRC counterparts also plan to use the stabilized spike protein as a probe to isolate naturally produced antibodies from people who’ve recovered from COVID-19. Such antibodies might form the basis of a treatment for people who’ve been exposed to the virus, such as health care workers.
The NIAID is now working with the biotechnology company Moderna, Cambridge, MA, to use the latest findings to develop a vaccine candidate using messenger RNA (mRNA), molecules that serve as templates for making proteins. The goal is to direct the body to produce a spike protein in such a way to elicit an immune response and the production of antibodies. An early clinical trial of the vaccine in people is expected to begin in the coming weeks. Other vaccine candidates are also in preclinical development.
Meanwhile, the first clinical trial in the U.S. to evaluate an experimental treatment for COVID-19 is already underway at the University of Nebraska Medical Center’s biocontainment unit [3]. The NIH-sponsored trial will evaluate the safety and efficacy of the experimental antiviral drug remdesivir in hospitalized adults diagnosed with COVID-19. The first participant is an American who was repatriated after being quarantined on the Diamond Princess cruise ship in Japan.
As noted, the risk of contracting COVID-19 in the United States is currently low, but the situation is changing rapidly. One of the features that makes the virus so challenging to stay in front of is its long latency period before the characteristic flu-like fever, cough, and shortness of breath manifest. In fact, people infected with the virus may not show any symptoms for up to two weeks, allowing them to pass it on to others in the meantime. You can track the reported cases in the United States on the Centers for Disease Control and Prevention’s website.
As the outbreak continues over the coming weeks and months, you can be certain that NIH and other U.S. public health organizations are working at full speed to understand this virus and to develop better diagnostics, treatments, and vaccines.
References:
[1] Cryo-EM structure of the 2019-nCoV spike in the prefusion conformation. Wrapp D, Wang N, Corbett KS, Goldsmith JA, Hsieh CL, Abiona O, Graham BS, McLellan JS. Science. 2020 Feb 19.
[2] A new coronavirus associated with human respiratory disease in China. Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY, Yuan ML, Zhang YL, Dai FH, Liu Y, Wang QM, Zheng JJ, Xu L, Holmes EC, Zhang YZ. Nature. 2020 Feb 3.
[3] NIH clinical trial of remdesivir to treat COVID-19 begins. NIH News Release. Feb 25, 2020.
Links:
Coronaviruses (National Institute of Allergy and Infectious Diseases/NIH)
Coronavirus (COVID-19) (NIAID)
Coronavirus Disease 2019 (Centers for Disease Control and Prevention, Atlanta)
NIH Support: National Institute of Allergy and Infectious Diseases

I have to know where people can get such virus? How will this type of virus live in an open air? Does it have any Temperature Condition for its’ living? Or will this type of virus deteriorate in a certain rate of temperature? Or will Multiply for a certain rate of Temperature? So, that we will be prepare for this condition, etc …
As far as I have seen the virus is not partial to any specific temperature range. I came to this conclusion by looking at the cdc’s map of the corona virus. Someone I know works in a clinic and they had someone come in who believed they had corona, and they had to sanitize the room and leave it for a long time (i think it was 2 days maybe?) Viruses multiply within the human body by injecting themselves into a human’s cell and inserting their nuclei in order to start duplication. I can only assume that a virus will eventually die without a host, but thrive in a temperature that is similar to that of a human body or an animal’s body (aprx. 98.6°F) though I haven’t found any real evidence to back up that idea. The best preventative actions you can take are to thoroughly wash your hands with warm water, avoid crowded areas and sick people, and to cover your mouth when you cough if you do happen to get the virus. It is mostly spread through bodily fluids, like spit when you cough or snot when you sneeze, so these actions will help you to protect yourself as well as the people around you.
Dear Dr. Collins,
Why don’t you comment on this paper? Nature Medicine 2015, doi:10.1038/nm.3985
Many many thanks to those working on all aspects of this unbelievably complex problem. God speed.
Excellent Scientific update on COVID
Other than the experiment drug Remdesivir
Are there any other treatments or therapies in the
BARDA pipeline being approved for HHS funding.
And how much funding is available for treatment research and development??
I myself wonder if with a combination of treatments. Could include Electromagnetic pulse therapy to weaken the spikes this mutated virus uses to attach itself to the blood cells in the human body? Is this something being studied?
FIrst, I like to say thanks to University of Medicine for sending me links on the website about the virus its very educational. Futhermore, to be reading this post is the first sign of improvement. However, viruses of the nature is very much know to exist and be around for years. documents do show that and if the virus RNA, proteins and various of the areas around that crown isn’t handled with wisdom it could possibly replicate itself. the virus is clear after protein in the human body and in the body of mammals (animals). as a result, I am hoping for best outcome so this virus never repeats itself ever again and becomes stronger then the other 5 strains that are connected to it. In addition, breakthroughs are great, being wise in making sure the vaccination will work probably and safely is top priority. good luck Dr or Drs we all can say we need the best outcome in the world to save lives. This virus type needs to be stopped its clearly after protein cells in the human body. if the vaccine can protect the protein cells in the human body it might give a stronger defense to white blood cells to help fight off the virus and give it no breathing space to live in the human body at all. Lastly,I can understand with all the research from past present and now why a patient has to in isolation of 14 days it really makes absolute sense to do so. finally, again I hope for all the best so many lives shall be healed from the deadly virus. keep up the great success!
That virus is horrible! Bless all of us!
Do you think there might be any potential role for the use of Angiotensin Receptor blockers to interfere with the attachment of the virus to the AT2 receptor?
I hope that companies receiving government support towards coronavirus vaccine development will be required to share data and work together. Each stage in vaccine development requires trial and error. The larger the effort and more complete the data sharing among the participants the less duplication there will be in things that are tried and not found fruitful, and the more quickly each stage can be completed, and the work moved to the next stage. The reward for the sharing, at the end of the day, would be that each company that took part in the coordinated effort would be licensed to produce and distribute the vaccine. No single company would get the entire market, but each would get a share.
This is truly amazing that science is now so advanced that this incredible detailed structural analysis of such tiny things is now possible, and can be done in such a short time! Congratulations to all involved.
The article referred to says that the spike proteins attach to ACE2 binding sites on epithelial cells. So my, perhaps ignorant, question is: would my blood pressure lowering ACE inhibitor medication ( I take rivaroxaban, for example), equip me with any degree of resistance to the virus, from blocking some of its attachment sites?
Might an inhalable formulation of an ACE inhibitor be useful as a treatment for this infection? Even if it only slowed it down, that might be enough for our immune systems to catch up with it.
Another idea I thought of, was that you could ask the hand sanitiser manufacturers to put bitter and bad smelling additives into their ‘Purell’ products for the time being? An unpleasant smell and taste would help break the habits of both hand shaking and of touching the face, eyes, and mouth. Must be worth a try.
Another thing I would suggest, is that you encourage Americans to bow to each other like the Japanese instead of shaking hands. This might even reduce the general level of community acquired infections in the US. Do you think it might also be why the Japanese tend to live longer? It might be as simple as not having the habit of shaking hands! …
Lowering your blood pressure will not slow the virus’s abilities. The most common way for your body to lower blood pressure is for the vessels to dilate. Your medication would be ineffective. Epithelial cells are all over your body, so even if it did have an effect, your blood would more than likely just carry it to a capillary that would then release it elsewhere in your body. The best preventative actions you can take are washing your hands thoroughly, and avoiding crowded areas and sick people.
I think Steve from England proposes a brilliant question regarding a potential side benefit of ACE inhibitors as a drug class. However, “ACE 2 is insensitive to classical small molecule inhibitors of human endothelial ACE such as captopril, lisinopril and enalaprilat” (Harmer, D., Gilbert, M., Borman, R. & Clark, K. L. Quantitative mRNA expression profiling of ACE 2, a novel homologue of angiotensin converting enzyme. FEBS Lett. 532, 107–110 (2002)).
Maybe we should be looking into ACE2 inhibitors?
With the advancement in Cryo-EM, discovery like these expedites the therapeutic and vaccine development. These would not be possible without the funding and support from NIH.
Since you touch on the types of coronaviruses, I wanted to point out that alpha coronaviruse (common cold) and beta-coronaviruses (COVID-19) have been shown to interact with cytoskeletal filaments (microtubule and actin filaments respectively) for internalization purposes. It has also been shown for some coronaviruses that targeting the cytoskeleton with tubulin or actin inhibitors reduces viral load.
This information can help build a new therapeutic strategy …
I thing your idea is best but it needs more time to solve it, on the base of genetics we should produce a recombine a gene that act as protein to prevent the internalization of (COVID-19)…
I hope will find a new vaccine as soon as.
I distrust vaccines to the point that I would literally rather die than ever get another one. I haven’t had the flu shot in over 18 years now, and “ironically”, I havent gotten the flu in over 18 years now… yet every person I know who did get the shot, got the flu. Sorry, maybe their problem-solving skills aren’t really that good…
In high temperature, corona virus can live? Or can’t?
Since one of the symptoms is high fever (increase in body temp) I would think they’d thrive in the heat. I would consider going the opposite direction as any atomic structure (electron orbit specifically) slows in the cold. IMO
I’m a laymen re virus research. Have a few simple mechanical patents that’s all. But I was reading about these bats and how, because their body temperature can exceed 104-105 during flight, the virus has evolved to withstand these body temps. Just thinking as a simpleton, are there ways to safely raise a patient’s body temp above high fever levels without permanent cell and/or neurological damage? Or – have researchers looked at finding a way to lower the temperature tolerance of the proteins making up the virus structure? This probably sounds elementary and dumb to a viral researcher, but sometimes solutions come from non-Mensa members thinking simply about something.
Am I the only one asking why the only reported cases of the virus are in humans and no other species? That’s a red flag for me as it then would appear to be manufactured to only attack human cells. Also, why is every country reporting cases of infection except one, North Korea. You would think the closest country to the 4th highest infected country would have at least one case. Could they have manufactured it and an antigen? Just curious. I have many more questions, but don’t want to sound like a conspiracy theory nutcase. Have you also looked into ultrasonic or infrared treatments on the cells? What about lowering pH or treating cells with Ammonium Chloride. Just asking.
Have the reasearchers tried the strategy called RNA interference for the development of vaccine for COVID19??
In this case, I was not referring to the blood pressure reduction as affecting the virus: I was referring to the ACE inhibitors (and similar drugs) depriving the virus of binding sites, and thus giving the immune system more time to mount a defence before being overwhelmed by new virions.
Thanks for the extra info Aaron. It was only hearing about the structure and binding affinities of the viral spikes’ being evolved to take advantage of ACE that reminded me of the meds, and that I hadn’t heard of anyone discussing receptor blocking as a possible antiviral mechanism to exploit. I’m only a ‘lay witness’ to the science, but do see possibilities that seem to being missed, from time to time.
May god give us the cure! And for those people who are part of the development of the vaccine, you are our heroes!!
Eradication of COVID-19 by vaccine or virusostatic or virusocid should be our objective as individual and society. God bless all the people with immunity.
I am a researcher but I don’t understand why we don’t streamline the vaccine development during this time of national emergency. Why don’t we use killed or inactivated COVID-19 (by irradiation or UV) to inoculate people? It would be much faster and cheaper. Moderna’s use of mRNA vaccine is proprietary, cumbersome, and expensive. If anybody can help me understand, please reply.
Vaccine design is very complicated, you have to understand how to elicit effective protective immunity in the human body. Antibodies generated from inactive viruses are strain specific and are effective due to highly conserved regions in some viruses. Constant genetic mutation in viral and within a single individual’s DNA present over a million variants- making the virus a moving target. That’s just one challenge, a major feature analyzed in vaccine design, especially with COVID-19 type viruses, is viral envelopes. COVID-19 has a spiked surface composed of a trimer(3 different proteins) to increase facilitation into the host cell AND is heavily glycosylated with host-derived carbohydrates masking recognition by the immune system. Given the window of opportunity to effectively neutralize viruses with antibodies, a more effective method is to find a way to modify the surface structure with probes that would allow detection for designing vaccines, or as “targets” for mapping edits like CRISPR
I commend the efforts of those working tirelessly to find a cure to this virus.
Since the reported covid-19 is closely related to SARS, Biotechnology centers should try possibilities of modifying SARS vaccine to meet the standard of the COVID-19.