CTE
New Findings in Football Players May Aid the Future Diagnosis and Study of Chronic Traumatic Encephalopathy (CTE)
Posted on by Dr. Monica M. Bertagnolli
Repeated hits to the head—whether from boxing, playing American football or experiencing other repetitive head injuries—can increase someone’s risk of developing a serious neurodegenerative condition called chronic traumatic encephalopathy (CTE). Unfortunately, CTE can only be diagnosed definitively after death during an autopsy of the brain, making it a challenging condition to study and treat. The condition is characterized by tau protein building up in the brain and causes a wide range of problems in thinking, understanding, impulse control, and more. Recent NIH-funded research shows that, alarmingly, even young, amateur players of contact and collision sports can have CTE, underscoring the urgency of finding ways to understand, diagnose, and treat CTE.1
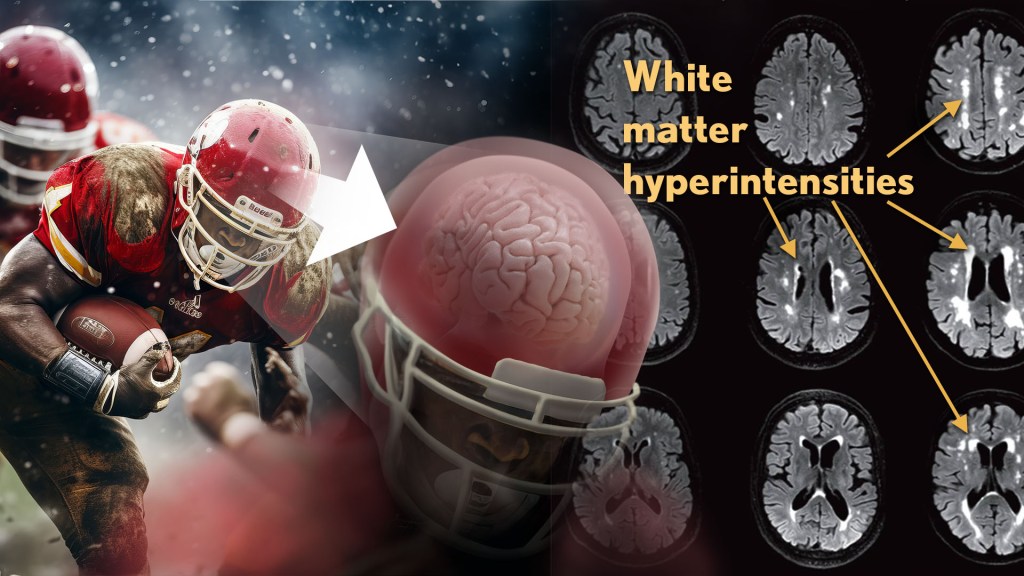
New findings published in the journal Neurology show that increased presence of certain brain lesions that are visible on MRI scans may be related to other brain changes in former football players. The study describes a new way to capture and analyze the long-term impacts of repeated head injuries, which could have implications for understanding signs of CTE. 2
The study analyzes data from the Diagnose CTE Research Project, an NIH-supported effort to develop methods for diagnosing CTE during life and to examine other potential risk factors for the degenerative brain condition. It involves 120 former professional football players and 60 former college football players with an average age of 57. For comparison, it also includes 60 men with an average age of 59 who had no symptoms, did not play football, and had no history of head trauma or concussion.
The new findings link some of the downstream risks of repetitive head impacts to injuries in white matter, the brain’s deeper tissue. Known as white matter hyperintensities (WMH), these injuries show up on MRI scans as easy-to-see bright spots.
Earlier studies had shown that athletes who had experienced repetitive head impacts had an unusual amount of WMH on their brain scans. Those markers, which also show up more as people age normally, are associated with an increased risk for stroke, cognitive decline, dementia and death. In the new study, researchers including Michael Alosco, Boston University Chobanian & Avedisian School of Medicine, wanted to learn more about WMH and their relationship to other signs of brain trouble seen in former football players.
All the study’s volunteers had brain scans and lumbar punctures to collect cerebrospinal fluid in search of underlying signs or biomarkers of neurodegenerative disease and white matter changes. In the former football players, the researchers found more evidence of WMH. As expected, those with an elevated burden of WMH were more likely to have more risk factors for stroke—such as high blood pressure, hypertension, high cholesterol, and diabetes—but this association was 11 times stronger in former football players than in non-football players. More WMH was also associated with increased concentrations of tau protein in cerebrospinal fluid, and this connection was twice as strong in the football players vs. non-football players. Other signs of functional breakdown in the brain’s white matter were more apparent in participants with increased WMH, and this connection was nearly quadrupled in the former football players.
These latest results don’t prove that WMH from repetitive head impacts cause the other troubling brain changes seen in football players or others who go on to develop CTE. But they do highlight an intriguing association that may aid the further study and diagnosis of repetitive head impacts and CTE, with potentially important implications for understanding—and perhaps ultimately averting—their long-term consequences for brain health.
References:
[1] AC McKee, et al. Neuropathologic and Clinical Findings in Young Contact Sport Athletes Exposed to Repetitive Head Impacts. JAMA Neurology. DOI:10.1001/jamaneurol.2023.2907 (2023).
[2] MT Ly, et al. Association of Vascular Risk Factors and CSF and Imaging Biomarkers With White Matter Hyperintensities in Former American Football Players. Neurology. DOI: 10.1212/WNL.0000000000208030 (2024).
NIH Support: National Institute of Neurological Disorders and Stroke, National Institute on Aging and the National Center for Advancing Translational Sciences
Brain Imaging: Tackling Chronic Traumatic Encephalopathy
Posted on by Dr. Francis Collins

Caption: Left to right, brain PET scans of healthy control; former NFL player with suspected chronic traumatic encephalopathy (CTE); and person with Alzheimer’s disease (AD). Areas with highest levels of abnormal tau protein appear red/yellow; medium, green; and lowest, blue.
Credit: Adapted from Barrio et al., PNAS
If you follow the National Football League (NFL), you may have heard some former players describe their struggles with a type of traumatic brain injury called chronic traumatic encephalopathy (CTE). Known to be associated with repeated, hard blows to the head, this neurodegenerative disorder can diminish the ability to think critically, slow motor skills, and lead to volatile, even suicidal, mood swings. What’s doubly frustrating to both patients and physicians is that CTE has only been possible to diagnose conclusively after death (via autopsy) because it’s indistinguishable from many other brain conditions with current imaging methods.
But help might be starting to move out of the backfield toward the goal line of more accurate diagnosis. In findings published in the journal PNAS [1], NIH-supported scientists from the University of California, Los Angeles (UCLA) and the University of Chicago report they’ve made some progress toward imaging CTE in living people. Following up on their preliminary work published in 2013 [2], the researchers used a specially developed radioactive tracer that lights up a neural protein, called tau, known to deposit in certain areas of the brain in individuals with CTE. They used this approach on PET scans of the brains of 14 former NFL players suspected of having CTE, generating maps of tau distribution throughout various regions of the brain.

