genotype
All of Us: Partnering Together for the Future of Precision Medicine
Posted on by Dr. Francis Collins

Over the past year, it’s been so inspiring to watch tens of thousands of people across the country selflessly step forward for vaccine trials and other research studies to combat COVID-19. And they are not alone. Many generous folks are volunteering to take part in other types of NIH-funded research that will improve health all across the spectrum, including the more than 360,000 who’ve already enrolled in the pioneering All of Us Research Program.
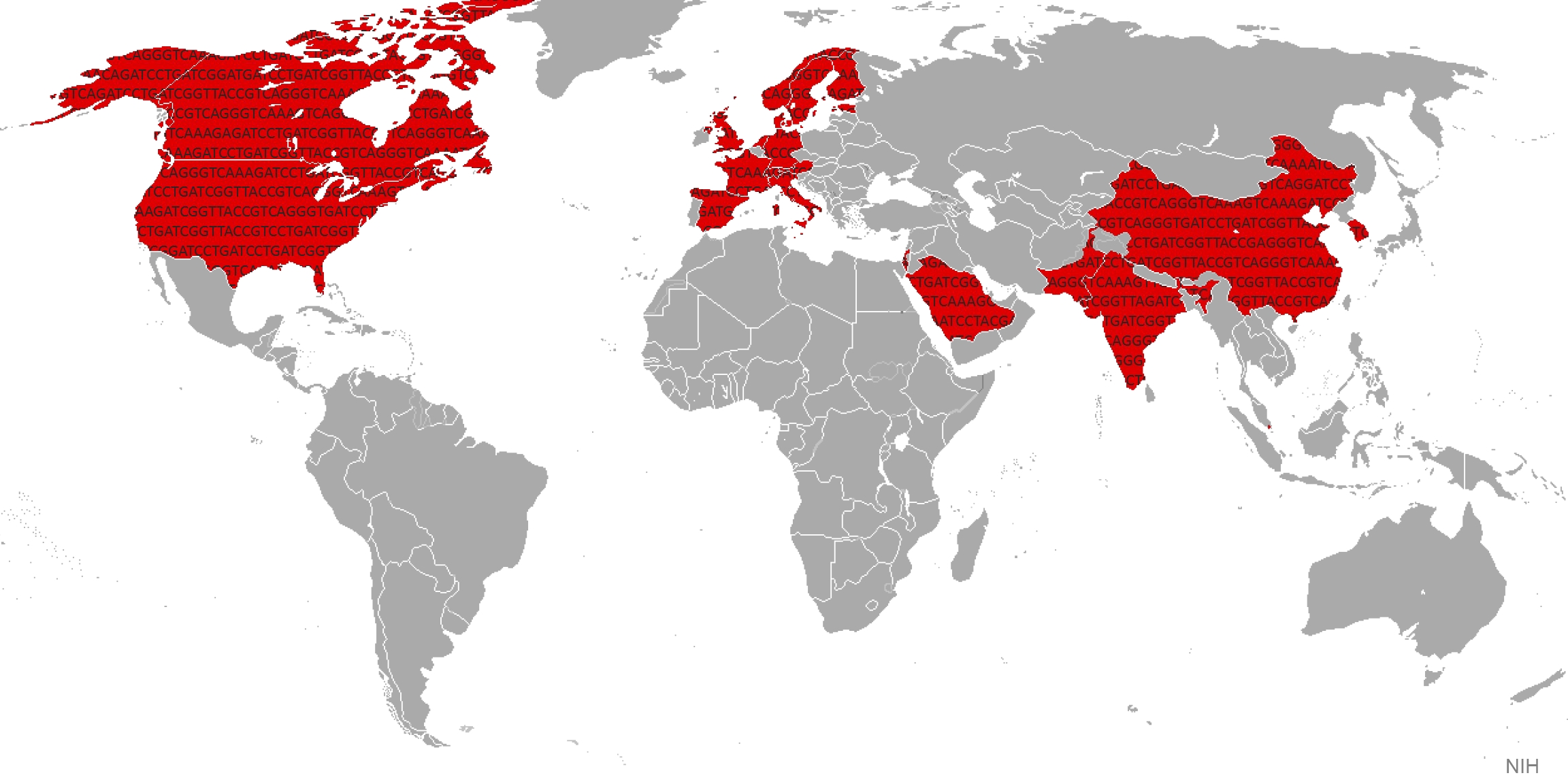
Now in its second year, All of Us is building a research community of 1 million participant partners to help us learn more about how genetics, environment, and lifestyle interact to influence disease and affect health. So far, more than 80 percent of participants who have completed all the initial enrollment steps are Black, Latino, rural, or from other communities historically underrepresented in biomedical research.
This community will build a diverse foundation for precision medicine, in which care is tailored to the individual, not the average patient as is now often the case. What’s also paradigm shifting about All of Us is its core value of sharing information back with participants about themselves. It is all done responsibly through each participant’s personal All of Us online account and with an emphasis on protecting privacy.
All of Us participants share their health information in many ways, such as taking part in surveys, offering access to their electronic health records, and providing biosamples (blood, urine, and/or saliva). In fact, researchers recently began genotyping and sequencing the DNA in some of those biosamples, and then returning results from analyses to participants who’ve indicated they’d like to receive such information. This first phase of genotyping DNA analysis will provide insights into their genetic ancestry and four traits, including bitter taste perception and tolerance for lactose.
Results of a second sequencing phase of DNA analysis will likely be ready in the coming year. These personalized reports will give interested participants information about how their bodies are likely to react to certain medications and about whether they face an increased risk of developing certain health conditions, such as some types of cancer or heart disease. To help participants better understand the results, they can make a phone appointment with a genetic counselor who is affiliated with the program.
This week, I had the pleasure of delivering the keynote address at the All of Us Virtual Face-to-Face. This lively meeting was attended by a consortium of more than 2,000 All of Us senior staff, program leads with participating healthcare provider organizations and federally qualified health centers, All of Us-supported researchers, community partners, and the all-important participant ambassadors.
If you are interested in becoming part of the All of Us community, I welcome you—there’s plenty of time to get involved! To learn more, just go to Join All of Us.
Links:
All of Us Research Program (NIH)
Join All of Us (NIH)
Gene Duplication: New Analysis Shows How Extra Copies Split the Work
Posted on by Dr. Francis Collins
 The human genome contains more than 20,000 protein-coding genes, which carry the instructions for proteins essential to the structure and function of our cells, tissues and organs. Some of these genes are very similar to each other because, as the genomes of humans and other mammals evolve, glitches in DNA replication sometimes result in extra copies of a gene being made. Those duplicates can be passed along to subsequent generations and, on very rare occasions, usually at a much later point in time, acquire additional modifications that may enable them to serve new biological functions. By starting with a protein shape that has already been fine-tuned for one function, evolution can produce a new function more rapidly than starting from scratch.
The human genome contains more than 20,000 protein-coding genes, which carry the instructions for proteins essential to the structure and function of our cells, tissues and organs. Some of these genes are very similar to each other because, as the genomes of humans and other mammals evolve, glitches in DNA replication sometimes result in extra copies of a gene being made. Those duplicates can be passed along to subsequent generations and, on very rare occasions, usually at a much later point in time, acquire additional modifications that may enable them to serve new biological functions. By starting with a protein shape that has already been fine-tuned for one function, evolution can produce a new function more rapidly than starting from scratch.
Pretty cool! But it leads to a question that’s long perplexed evolutionary biologists: Why don’t duplicate genes vanish from the gene pool almost as soon as they appear? After all, instantly doubling the amount of protein produced in an organism is usually a recipe for disaster—just think what might happen to a human baby born with twice as much insulin or clotting factor as normal. At the very least, duplicate genes should be unnecessary and therefore vulnerable to being degraded into functionless pseudogenes as new mutations arise over time
An NIH-supported team offers a possible answer to this question in a study published in the journal Science. Based on their analysis of duplicate gene pairs in the human and mouse genomes, the researchers suggest that extra genes persist in the genome because of rapid changes in gene activity. Instead of the original gene producing 100 percent of a protein in the body, the gene duo quickly divvies up the job [1]. For instance, the original gene might produce roughly 50 percent and its duplicate the other 50 percent. Most importantly, organisms find the right balance and the duplicate genes can easily survive to be passed along to their offspring, providing fodder for continued evolution.