Epstein-Barr
Study Reveals How Epstein-Barr Virus May Lead to Cancer
Posted on by Lawrence Tabak, D.D.S., Ph.D.
Chances are good that you’ve had an Epstein-Barr virus (EBV) infection, usually during childhood. More than 90 percent of us have, though we often don’t know it. That’s because most EBV infections are mild or produce no symptoms at all.
But in some people, EBV can lead to other health problems. The virus can cause infectious mononucleosis (“mono”), type 1 diabetes, and other ailments. It also can persist in our bodies for years and cause increased risk later in life for certain cancers, such as lymphoma, leukemia, and head and neck cancer. Now, an NIH-funded team has some of the best evidence yet to explain how this EBV that hangs around may lead to cancer [1].
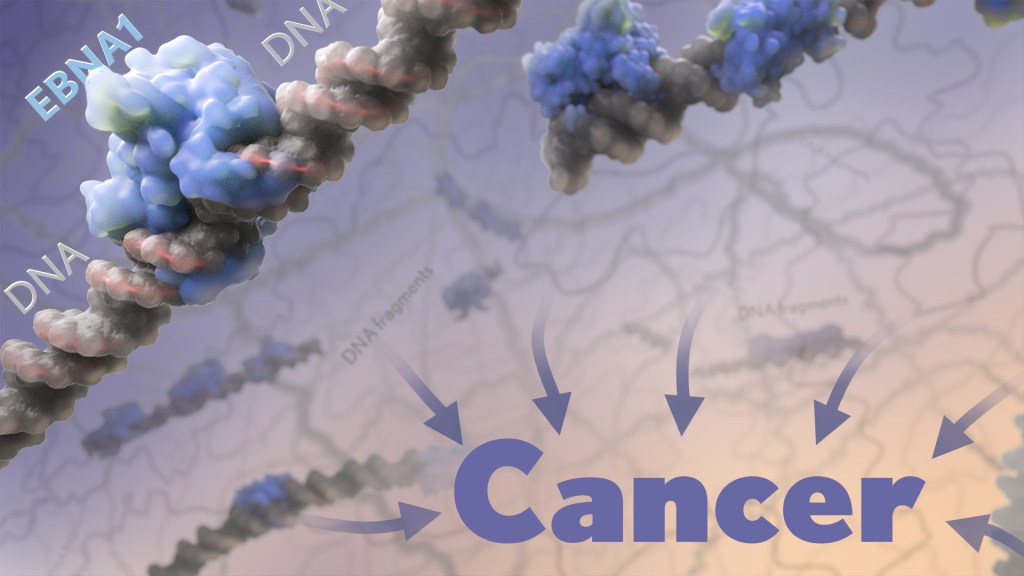
The paper, published recently in the journal Nature, shows that a key viral protein readily binds to a particular spot on a particular human chromosome. Where the protein accumulates, the chromosome becomes more prone to breaking for reasons that aren’t yet fully known. What the study makes clearer is that the breakage produces latently infected cells that are more likely over time to become cancerous.
This discovery paves the way potentially for ways to screen for and identify those at particular risk for developing EBV-associated cancers. It may also fuel the development of promising new ways to prevent these cancers from arising in the first place.
The work comes from a team led by Don Cleveland and Julia Su Zhou Li, University of California San Diego’s Ludwig Cancer Research, La Jolla, CA. Over the years, it’s been established that EBV, a type of herpes virus, often is detected in certain cancers, particularly in people with a long-term latent infection. What interested the team is a viral protein, called EBNA1, which routinely turns up in those same EBV-related cancers.
The EBNA1 protein is especially interesting because it binds viral DNA in particular spots, which allows the virus to persist and make more copies of itself. This discovery raised the intriguing possibility that the protein may also bind similar sequences in human DNA. While it had been suggested previously that this interaction might play a role in EBV-associated cancers, the details had remained murky—until now.
In the new study, the researchers first made uninfected human cells produce the viral EBNA1 protein. They then peered inside them with a microscope to see where those proteins went. In both healthy and cancerous human cells, they watched as EBNA1 proteins built up at two distinct spots and confirmed that this accumulation was dependent on the protein’s ability to bind DNA.
Next, they mapped where exactly EBNA1 binds to human DNA. Interestingly, it was along a repetitive non-protein-coding stretch of DNA on human chromosome 11. This region includes more than 300 copies of an 18-letter sequence that looks quite similar to the EBNA1-binding sites in its own viral genome.
What’s more, the researchers noticed that the repetitive DNA there takes on a structure that’s known for being unstable. And these so-called fragile sites are inherently prone to breaking.
The team went on to uncover evidence that the buildup of EBNA1 at this already fragile site only makes matters worse. In EBV-infected cells, increasing the amount of EBNA1 protein led to more chromosome 11 breaks. Those breaks showed up within a single day in about 40 percent of cells.
For these cells, those breaks also may be a double whammy. That’s because the breaks are located next to neighboring genes with long recognized roles in regulating cell growth. When altered, these genes can contribute to turning a cell cancerous.
To further nail down the link to cancer, the researchers looked to whole-genome sequencing data for more than 2,400 cancers including 38 tumor types from the international Pan-Cancer Analysis of Whole Genomes consortium [2]. They found that tumors with detectable EBV also had an unusually high number of chromosome 11 abnormalities. In fact, that was true in every single case of head and neck cancer.
The findings suggest that people will vary in their susceptibility to EBNA1-induced DNA breaks along chromosome 11 based on the amount of EBNA1 protein in their latently infected cells. It also will depend on the number of EBV-like DNA repeats present in their DNA.
Given these new findings, it’s worth noting that the presence of EBV and the very same viral protein has been implicated also in the link between EBV and multiple sclerosis (MS) [3]. Together, these recent findings are a reminder of the value in pursuing an EBV vaccine that might thwart this infection and its associated conditions, including certain cancers and MS. And, we’re getting there. In fact, an early-stage clinical trial for an experimental EBV vaccine is now ongoing here at the NIH Clinical Center.
References:
[1] Chromosomal fragile site breakage by EBV-encoded EBNA1 at clustered repeats. Li JSZ, Abbasi A, Kim DH, Lippman SM, Alexandrov LB, Cleveland DW. Nature. 2023 Apr 12.
[2] Pan-cancer analysis of whole genomes. ICGC/TCGA Pan-Cancer Analysis of Whole Genomes Consortium. Nature.2020 Feb;578(7793):82-93.
[3] Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Lanz TV, Brewer RC, Steinman L, Robinson WH, et al. Nature. 2022 Mar;603(7900):321-327.
Links:
About Epstein-Barr Virus (Centers for Disease Control and Prevention, Atlanta)
Head and Neck Cancer (National Cancer Institute,/NIH)
Multiple Sclerosis (National Institute of Neurological Disorders and Stroke/NIH)
Don W. Cleveland Lab (University of California San Diego, La Jolla, CA)
NIH Support: National Institute of General Medical Sciences; National Institute of Environmental Health Sciences; National Cancer Institute
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
A Look Back at Science’s 2022 Breakthroughs
Posted on by Lawrence Tabak, D.D.S., Ph.D.
Happy New Year! I hope everyone finished 2022 with plenty to celebrate, whether it was completing a degree or certification, earning a promotion, attaining a physical fitness goal, or publishing a hard-fought scientific discovery.
If the latter, you are in good company. Last year produced some dazzling discoveries, and the news and editorial staff at the journal Science kept a watchful eye on the most high-impact advances of 2022. In December, the journal released its list of the top 10 advances across the sciences, from astronomy to zoology. In case you missed it, Science selected NASA’s James Webb Space Telescope (JWST) as the 2022 Breakthrough of the Year [1].
This unique space telescope took 20 years to complete, but it has turned out to be time well spent. Positioned 1.5-million-kilometers from Earth, the JWST and its unprecedented high-resolution images of space have unveiled the universe anew for astronomers and wowed millions across the globe checking in online. The telescope’s image stream, beyond its sheer beauty, will advance study of the early Universe, allowing astronomers to discover distant galaxies, explore the early formation of stars, and investigate the possibility of life on other planets.
While the biomedical sciences didn’t take home the top prize, they were well represented among Science’s runner-up breakthroughs. Some of these biomedical top contenders also have benefited, directly or indirectly, from NIH efforts and support. Let’s take a look:
RSV vaccines nearing the finish line: It’s been one of those challenging research marathons. But scientists last year started down the homestretch with the first safe-and-effective vaccine for respiratory syncytial virus (RSV), a leading cause of severe respiratory illness in the very young and the old.
In August, the company Pfizer presented evidence that its experimental RSV vaccine candidate offered protection for those age 60 and up. Later, they showed that the same vaccine, when administered to pregnant women, helped to protect their infants against RSV for six months after birth. Meanwhile, in October, the company GSK announced encouraging results from its late-stage phase III trial of an RSV vaccine in older adults.
As Science noted, the latest clinical progress also shows the power of basic science. For example, researchers have been working with chemically inactivated versions of the virus to develop the vaccine. But these versions have a key viral surface protein that changes its shape after fusing with a cell to start an infection. In this configuration, the protein elicits only weak levels of needed protective antibodies.
Back in 2013, Barney Graham, then with NIH’s National Institute of Allergy and Infectious Diseases (NIAID), and colleagues, solved the problem [2]. Graham’s NIH team discovered a way to lock the protein into its original prefusion state, which the immune system can better detect. This triggers higher levels of potent antibodies, and the discovery kept the science—and the marathon—moving forward.
These latest clinical advances come as RSV and other respiratory viruses, including SARS-CoV-2, the cause of COVID-19, are sending an alarming number of young children to the hospital. The hope is that researchers will cross the finish line this year or next, and we’ll have the first approved RSV vaccine.
Virus fingered as cause of multiple sclerosis: Researchers have long thought that multiple sclerosis, or MS, has a viral cause. Pointing to the right virus with the required high degree of certainty has been the challenge, slowing progress on the treatment front for those in need. As published in Science last January, Alberto Ascherio, Harvard T.H. Chan School of Public Health, Boston, and colleagues produced the strongest evidence yet that MS is caused by the Epstein-Barr virus (EBV), a herpesvirus also known for causing infectious mononucleosis [3].
The link between EBV and MS had long been suspected. But it was difficult to confirm because EBV infections are so widespread, and MS is so disproportionately rare. In the recent study, the NIH-supported researchers collected blood samples every other year from more than 10 million young adults in the U.S. military, including nearly 1,000 who were diagnosed with MS during their service. The evidence showed that the risk of an MS diagnosis increased 32-fold after EBV infection, but it held steady following infection with any other virus. Levels in blood serum of a biomarker for MS neurodegeneration also went up only after an EBV infection, suggesting that the viral illness is a leading cause for MS.
Further evidence came last year from a discovery published in the journal Nature by William Robinson, Stanford University School of Medicine, Stanford, CA, and colleagues. The NIH-supported team found a close resemblance between an EBV protein and one made in the healthy brain and spinal cord [4]. The findings suggest an EBV infection may produce antibodies that mistakenly attack the protective sheath surrounding our nerve cells. Indeed, the study showed that up to one in four people with MS had antibodies that bind both proteins.
This groundbreaking research suggests that an EBV vaccine and/or antiviral drugs that thwart this infection might ultimately prevent or perhaps even cure MS. Of note, NIAID launched last May an early-stage clinical trial for an experimental EBV vaccine at the NIH Clinical Center, Bethesda, MD.
AI Gets Creative: Science’s 2021 Breakthrough of the Year was AI-powered predictions of protein structure. In 2022, AI returned to take another well-deserved bow. This time, Science singled out AI’s now rapidly accelerating entry into once uniquely human attributes, such as artistic expression and scientific discovery.
On the scientific discovery side, Science singled out AI’s continued progress in getting creative with the design of novel proteins for vaccines and myriad other uses. One technique, called “hallucination,” generates new proteins from scratch. Researchers input random amino acid sequences into the computer, and it randomly and continuously mutates them into sequences that other AI tools are confident will fold into stable proteins. This greatly simplifies the process of protein design and frees researchers to focus their efforts on creating a protein with a desired function.
AI research now engages scientists around world, including hundreds of NIH grantees. Taking a broader view of AI, NIH recently launched the Artificial Intelligence/Machine Learning Consortium to Advance Health Equity and Researcher Diversity (AIM-AHEAD) Program. It will help to create greater diversity within the field, which is a must. A lack of diversity could perpetuate harmful biases in how AI is used, how algorithms are developed and trained, and how findings are interpreted to avoid health disparities and inequities for underrepresented communities.
And there you have it, some of the 2022 breakthroughs from Science‘s news and editorial staff. Of course, the highlighted biomedical breakthroughs don’t capture the full picture of research progress. There were many other milestone papers published in 2022 that researchers worldwide will build upon in the months and years ahead to make further progress in their disciplines and, for some, draw the attention of Science’s news and editorial staff. Here’s to another productive year in biomedical research, which the blog will continue to feature and share with you as it unfolds in 2023.
References:
[1] 2022 Breakthrough of the Year. Science. Dec 15, 2022.
[2] Structure of RSV fusion glycoprotein trimer bound to a prefusion-specific neutralizing antibody. McLellan JS, Chen M, Leung S, Kwong PD, Graham BS, et al. Science. 2013 May 31;340(6136):1113-1117.
[3] Longitudinal analysis reveals high prevalence of Epstein-Barr virus associated with multiple sclerosis. Bjornevik K, Cortese M, Healy BC, Kuhle J, Mina MJ, Leng Y, Elledge SJ, Niebuhr DW, Scher AI, Munger KL, Ascherio A. Science. 2022 Jan 21;375(6578):296-301.
[4] Clonally expanded B cells in multiple sclerosis bind EBV EBNA1 and GlialCAM. Lanz TV, Brewer RC, Steinman L, Robinson WH, et al. Nature. 2022 Mar;603(7900):321-327.
Links:
Respiratory Syncytial Virus (RSV) (National Institute of Allergy and Infectious Diseases/NIH)
Multiple Sclerosis (National Institute of Neurological Disorders and Stroke/NIH)
Barney Graham (Morehouse School of Medicine, Atlanta)
Alberto Ascherio (Harvard T.H. Chan School of Public Health, Boston)
Robinson Lab (Stanford Medicine, Stanford, CA)
James Webb Space Telescope (Goddard Space Flight Center/NASA, Greenbelt, MD)
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Posted In: News
Tags: 2022 Science Breakthrough of the Year, AI, AI Hallucination, AIM-AHEAD, basic research, Creative AI, EBV, EBV vaccine, Epstein-Barr, GSK, health disparities, James Webb Space Telescope, JWST, machine learning, MS, multiple sclerosis, NIH Clinical Center, Pfizer, respiratory syncytial virus, RSV, RSV vaccine, SARS-CoV-2, vaccine, virus
Summer Reading Suggestions from Scientists: Robert Horvitz
Posted on by Dr. Robert Horvitz
 Two Science Selections:
Two Science Selections:
Horace Freeland Judson, Eighth Day of Creation. A comprehensive history of the origins and early science of the field of modern molecular biology, written by historian Horace Freeland Judson based on personal interviews with those who drove the revolution in biology. First and foremost are the science—DNA, RNA and protein, the genetic code, and gene regulation—and the scientific process—the seed ideas, the “aha” insights and the brilliant and elegant experiments. But this book is also the story of scientists in the process of discovery and of how the science that emerged was at least as much a consequence of the personalities as of the experimental skills of those involved. Fascinating, engaging, and fun—I’ve recommended this book to many, scientist and non-scientist alike.
Georgina Ferry, Dorothy Hodgkin. A superb biography of one of modern science’s most exceptional and distinguished pioneers. Awarded the Nobel Prize in Chemistry in 1964 for determining the crystal structures of penicillin and vitamin B12, Dorothy Crowfoot Hodgkin faced repeated challenges as a woman attempting to study and then pursue a career in chemistry in the 1930s and 1940s in England. Hodgkin is only one of four women ever awarded the Nobel Prize in Chemistry; the others were Marie Curie (1911); her daughter Irene Joliot-Curie (1935); and Ada Yonath (2009). Once recognized, Hodgkin worked hard to combat social inequalities and was president for more than a decade of Pugwash, an international organization founded by Bertrand Russell and dedicated to preventing war. Hodgkin has been a role model for many, although she disagreed rather strongly with the political views and actions of her most famous student, Margaret Thatcher.
Personal Connection:
George Klein, The Atheist and the Holy City. This book was a gift to me from George Klein, a Hungarian-Swedish tumor biologist and virologist at the Karolinska Institute in Stockholm. George and his wife Eva are best known in biological circles for their pioneering discovery of the role of the Epstein-Barr virus in Burkitt’s lymphoma and other neoplasms. This book, one of many George has written, is a compilation of essays that focus on science, but incorporate history, religion and philosophy. Its sections are entitled “The Wisdom and Folly of Scientists,” “Journeys,” “Viruses and Cancer” and “The Human Condition,” and collectively touch upon topics as diverse as DNA hybridization, the discovery of Rous sarcoma virus, and the life cycle of Schistosoma mansoni, as well as the Nazi death camps, scientific creativity, and the conviction that God is an example of man’s wishful thinking. Thought-provoking and uplifting, this book is a story of science and much more. A must read for all.![]()
Robert Horvitz, Ph.D. is the David H. Koch Professor of Biology at the Massachusetts Institute of Technology, and a member of the MIT McGovern Institute for Brain Research and the MIT Koch Institute for Integrative Cancer Research. Dr. Horvitz is co-winner of the 2002 Nobel Prize in Physiology or Medicine for discoveries concerning genetic regulation of organ development and programmed cell death.
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Posted In: books, Health, Science
Tags: Ada Yonath, Bertrand Russell, books, Dorothy Hodgkin, Eighth Day of Creation, Epstein-Barr, George Klein, Georgina Ferry, history, Horace Freeland Judson, Irene Joliot-Curie, Karolinska Institute, lymphoma, Margaret Thatcher, Marie Curie, molecular biology, Nazi, Nobel Prize, penicillin, philosophy, Pugwash, religion, Rous sarcoma, Schistosoma mansoni, summer books, summer reading, The Atheist and the Holy City, virus, vitamin B12