How One Change to The Coronavirus Spike Influences Infectivity
Posted on by Lawrence Tabak, D.D.S., Ph.D.
Since joining NIH, I’ve held a number of different leadership positions. But there is one position that thankfully has remained constant for me: lab chief. I run my own research laboratory at NIH’s National Institute of Dental and Craniofacial Research (NIDCR).
My lab studies a biochemical process called O-glycosylation. It’s fundamental to life and fascinating to study. Our cells are often adorned with a variety of carbohydrate sugars. O-glycosylation refers to the biochemical process through which these sugar molecules, either found at the cell surface or secreted, get added to proteins. The presence or absence of these sugars on certain proteins plays fundamental roles in normal tissue development and first-line human immunity. It also is associated with various diseases, including cancer.
Our lab recently joined a team of NIH scientists led by my NIDCR colleague Kelly Ten Hagen to demonstrate how O-glycosylation can influence SARS-CoV-2, the coronavirus that causes COVID-19, and its ability to fuse to cells, which is a key step in infecting them. In fact, our data, published in the journal Proceedings of the National Academy of Sciences, indicate that some variants, seem to have mutated to exploit the process to their advantage [1].
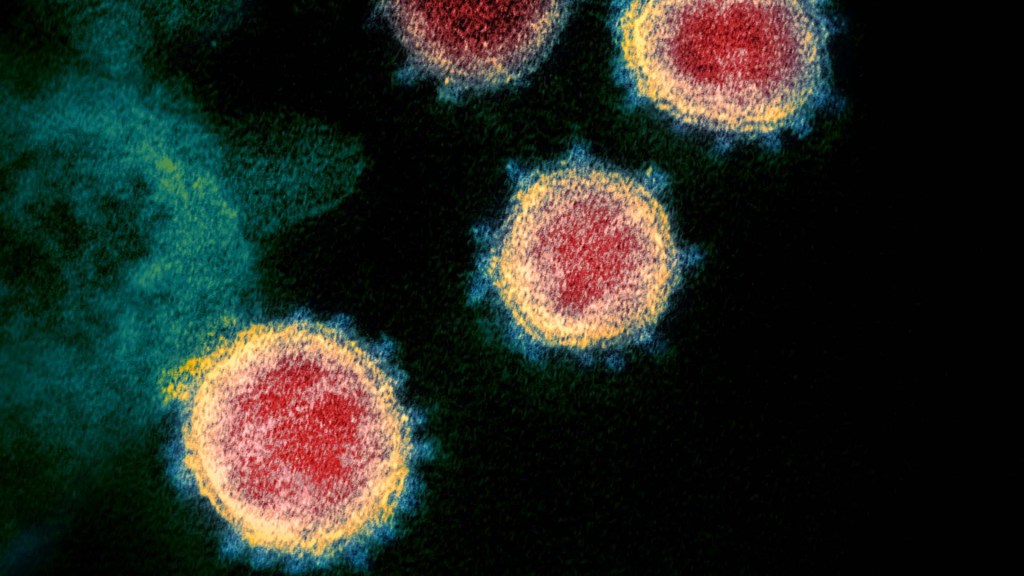
The work builds on the virus’s reliance on the spike proteins that crown its outer surface to attach to human cells. Once there, the spike protein must be activated to fuse and launch an infection. That happens when enzymes produced by our own cells make a series of cuts, or cleavages, to the spike protein.
The first cut comes from an enzyme called furin. We and others had earlier evidence that O-glycosylation can affect the way furin makes those cuts. That got us thinking: Could O-glycosylation influence the interaction between furin and the spike protein? The furin cleavage area of the viral spike was indeed adorned with sugars, and their presence or absence might influence spike activation by furin.
We also noticed the Alpha and Delta variants carry a mutation that removes the amino acid proline in a specific spot. That was intriguing because we knew from earlier work that enzymes called GALNTs, which are responsible for adding bulky sugar molecules to proteins, prefer prolines near O-glycosylation sites.
It also suggested that loss of proline in the new variants could mean decreased O-glycosylation, which might then influence the degree of furin cleavage and SARS-CoV-2’s ability to enter cells. I should note that the recent Omicron variant was not examined in the current study.
After detailed studies in fruit fly and mammalian cells, we demonstrated in the original SARS-CoV-2 virus that O-glycosylation of the spike protein decreases furin cleavage. Further experiments then showed that the GALNT1 enzyme adds sugars to the spike protein and this addition limits the ability of furin to make the needed cuts and activate the spike protein.
Importantly, the spike protein change found in the Alpha and Delta variants lowers GALNT1 activity, making it easier for furin to start its activating cuts. It suggests that glycosylation of the viral spike by GALNT1 may limit infection with the original virus, and that the Alpha and Delta variant mutation at least partially overcomes this effect, to potentially make the virus more infectious.
Building on these studies, our teams looked for evidence of GALNT1 in the respiratory tracts of healthy human volunteers. We found that the enzyme is indeed abundantly expressed in those cells. Interestingly, those same cells also express the ACE2 receptor, which SARS-CoV-2 depends on to infect human cells.
It’s also worth noting here that the Omicron variant carries the very same spike mutation that we studied in Alpha and Delta. Omicron also has another nearby change that might further alter O-glycosylation and cleavage of the spike protein by furin. The Ten Hagen lab is looking into these leads to learn how this region in Omicron affects spike glycosylation and, ultimately, the ability of this devastating virus to infect human cells and spread.
Reference:
[1] Furin cleavage of the SARS-CoV-2 spike is modulated by O-glycosylation. Zhang L, Mann M, Syed Z, Reynolds HM, Tian E, Samara NL, Zeldin DC, Tabak LA, Ten Hagen KG. PNAS. 2021 Nov 23;118(47).
Links:
COVID-19 Research (NIH)
Kelly Ten Hagen (National Institute of Dental and Craniofacial Research/NIH)
Lawrence Tabak (NIDCR)
NIH Support: National Institute of Dental and Craniofacial Research

Most of us think of the increase in infections as a “spike”, ironic that such things are related to the “spike” proteins of the virus itself.
I more commonly hear and read of an increase in SARS-CoV-2 infections referred to as a “surge.”
As viruses are not alive, mutation is carried out on our ribosomes during transcription. There is an error checking mechanism and a repair mechanism. It seems to me that this virus can produce a molecule that defeats one or both. Has anyone looked at this? It could be a path to a therapy that reduces point mutations.
Codon usage with pseudo-uridine allows for wobble. And mRNA viruses bypass proof-reading functions. One of the major issues when large pharmaceutical companies were looking into developing HIV vaccines. Scientific literature from over a decade ago is not necessarily obsolete.
I thank Director Dr. Tabak for highlighting this complex aspect of the chess game against the SARS-CoV-2 virus, to understand the mechanisms of the infection.
The nebulization of Glutathione and N-Acetylcysteine (NAC) it is proposed by some Authors as an adjuvant therapy for COVID-19 onset. Could the explanation of the therapeutic action of NAC, in addition to those already recognized deriving from the many years of use of NAC for respiratory diseases, also be linked to the action on the molecular mechanisms highlighted in your study? NAC plays a different role, depending on the SARS-CoV-2 variants?
Since Ivermectin has been in a government trial, that started June 8, 2021 and is on going as a phase 3 trial. I believe that if the trial was not going well, the trial would have been stopped. Do you agree?
I presume you’re referring to the study headed by Susanna Naggie, MD out of Duke, NCT04885530?
If so, that study also is evaluating fluvoxamine and fluticasone as well as ivermectin (and is placebo-controlled, of course). They may not have enough data at this point to know if the trial of ivermectin (and other tested medications) is or is not going well. The estimated completion date of that study isn’t until March 2023.
Reading the many articles produced by the Director and his team on this biochemical topic, one understands the importance of this scientific sector so complex and fundamental for the tissues and organs of the whole body . An eg. : Revoredo, L., Wang, S., Bennett, E. P., Clausen, H., Moremen, K. W., Jarvis, D. L., Ten Hagen, K. G., Tabak, L. A., & Gerken, T. A. (2016). Mucin-type O-glycosylation is controlled by short- and long-range glycopeptide substrate recognition that varies among members of the polypeptide GalNAc transferase family. Glycobiology, 26(4), 360–376.
Regarding glycoproteins called mucins, in the complex mechanism of interaction with the Spike protein, how important is the role of the microbiota in the final outcome of the infection for each individual? In the ways where the virus can enter, we know that the eye, the mucous membrane of the digestive tract (starting from the mouth) and that of the upper airways, all have their own microbiota and a system of protective substances for defense against external aggressors.
Hansson G. C. (2020). Mucins and the Microbiome. Annual review of biochemistry, 89, 769–793.
Microbiota and Covid19: another question arise. Does the microbiota affect the course of the Covid19 disease or is it Covid19 that causes a harmful microbiota to emerge? Or can both correlations be true simultaneously, conditioning each other in a negative vortex?
Woodall CA, McGeoch LJ, Hay AD, Hammond A. Respiratory tract infections and gut microbiome modifications: A systematic review. PLoS One. 2022 Jan 13;17(1):e0262057. doi: 10.1371/journal.pone.0262057. PMID: 35025938; PMCID: PMC8757905.
Ren Z, Wang H, Cui G, et al. Alterations in the human oral and gut microbiomes and lipidomics in COVID-19 Gut 2021;70:1253-1265.
Zuo T, Zhang F, Lui GCY, Yeoh YK, Li AYL, Zhan H, Wan Y, Chung ACK, Cheung CP, Chen N, Lai CKC, Chen Z, Tso EYK, Fung KSC, Chan V, Ling L, Joynt G, Hui DSC, Chan FKL, Chan PKS, Ng SC. Alterations in Gut Microbiota of Patients With COVID-19 During Time of Hospitalization. Gastroenterology. 2020 Sep;159(3):944-955.e8. doi: 10.1053/j.gastro.2020.05.048. Epub 2020 May 20. PMID: 32442562; PMCID: PMC7237927.
Can we interpret these phenomena comparing them to the tops of the trees of a forest, while the mucins with the modalities of glycosylation represent the undergrowth that feeds the roots?
Very pertinent point. The human body has more micro-organism cells than human cells co-existing in a symbiotic relationship. Why the aspect of immunity may differ widely between those living in crowded slums and barrios and those living in pristine mansions where the concept of “social distancing” and booster shots is commonly accepted. Why many interventions used in the developed world fail when transposed in societies that are less privileged. Every population is a distribution. What applies to one end of the distribution may not necessarily be valid for the other end. In a global pandemic, that population is 7+ billion, not the population of one continent or another. Tough conundrum since nothing really happens for “free”.
Thank you for your observations, which lead to evaluating concrete aspects. Probably, in a comfortable life situation there are factors favoring good health, better than in an environment of misery and deprivation.
The question :
the O-glycosylation can be quantitatively different depending on the person and in the same individual is expressed differently, related to some factors such as the microbiota?
The availability of foods, both the quantity and the quality, the way in which they are consumed, are the factors that influence the variability of genetic expression since, in addition to a direct biochemical action of the nutrients, they determine the composition of the microbiota.
In our life, are we always equally susceptible to gut-immunity crosstalk? Comparison studies on individual variations of the microbiota in relation to the changing global conditions (including economic ones) of the person would be interesting.
After all the Flu And Pneumonia and the Moderna mRNA two dose vaccine and my blood work came back * Anemic; not including the medication prescribed that was a Clinical Trial medication?!?!
Thank you for making us understand what difficulties each one can have in daily life, with different individual reactions to the same medical event. I’m not the most suitable person to be able to give answers to such a complex question.
We can observe that at a lunch: one person must avoid eating gluten because celiac, another cannot eat cheese because allergic, yet another absolutely avoids fava beans due to the danger of fatal hemolytic anemia.
Fascinating Covid-19 spike protein o-glycosylation biochemical odyssey!!! My scientific and clinical research interests were propelled further for demystifying the complex host-microbe interface cross-talks in spike-related mutation studies for stratifying Omicron vs Delta variants susceptible Covid-19 symptomatic as well as asymptomatic population subsets in the Covid-19 vaccination era.
How can I get inactivated viral culture supernates to test pathobiology hyposthesis. I need the released microsomes and protein/glycoprotein. Want virus inactivated to use in BSL2 lab
Thank you Dr Tabak for your informative article.