Can Autoimmune Antibodies Explain Blood Clots in COVID-19?
Posted on by Dr. Francis Collins
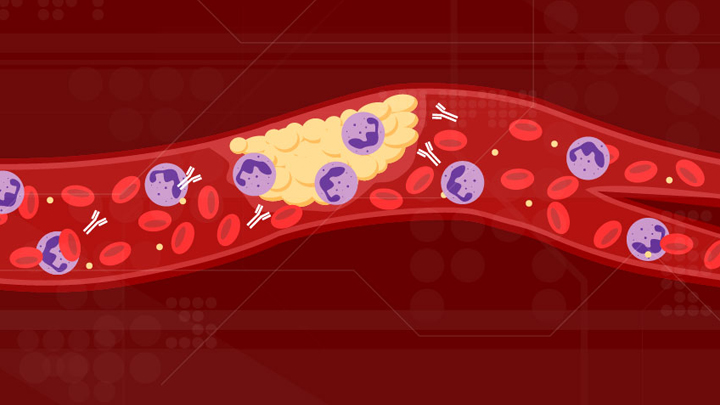
For people with severe COVID-19, one of the most troubling complications is abnormal blood clotting that puts them at risk of having a debilitating stroke or heart attack. A new study suggests that SARS-CoV-2, the coronavirus that causes COVID-19, doesn’t act alone in causing blood clots. The virus seems to unleash mysterious antibodies that mistakenly attack the body’s own cells to cause clots.
The NIH-supported study, published in Science Translational Medicine, uncovered at least one of these autoimmune antiphospholipid (aPL) antibodies in about half of blood samples taken from 172 patients hospitalized with COVID-19. Those with higher levels of the destructive autoantibodies also had other signs of trouble. They included greater numbers of sticky, clot-promoting platelets and NETs, webs of DNA and protein that immune cells called neutrophils spew to ensnare viruses during uncontrolled infections, but which can lead to inflammation and clotting. These observations, coupled with the results of lab and mouse studies, suggest that treatments to control those autoantibodies may hold promise for preventing the cascade of events that produce clots in people with COVID-19.
Our blood vessels normally strike a balance between producing clotting and anti-clotting factors. This balance keeps us ready to seal up vessels after injury, but otherwise to keep our blood flowing at just the right consistency so that neutrophils and platelets don’t stick and form clots at the wrong time. But previous studies have suggested that SARS-CoV-2 can tip the balance toward promoting clot formation, raising questions about which factors also get activated to further drive this dangerous imbalance.
To learn more, a team of physician-scientists, led by Yogendra Kanthi, a newly recruited Lasker Scholar at NIH’s National Heart, Lung, and Blood Institute and his University of Michigan colleague Jason S. Knight, looked to various types of aPL autoantibodies. These autoantibodies are a major focus in the Knight Lab’s studies of an acquired autoimmune clotting condition called antiphospholipid syndrome. In people with this syndrome, aPL autoantibodies attack phospholipids on the surface of cells including those that line blood vessels, leading to increased clotting. This syndrome is more common in people with other autoimmune or rheumatic conditions, such as lupus.
It’s also known that viral infections, including COVID-19, produce a transient increase in aPL antibodies. The researchers wondered whether those usually short-lived aPL antibodies in COVID-19 could trigger a condition similar to antiphospholipid syndrome.
The researchers showed that’s exactly the case. In lab studies, neutrophils from healthy people released twice as many NETs when cultured with autoantibodies from patients with COVID-19. That’s remarkably similar to what had been seen previously in such studies of the autoantibodies from patients with established antiphospholipid syndrome. Importantly, their studies in the lab further suggest that the drug dipyridamole, used for decades to prevent blood clots, may help to block that antibody-triggered release of NETs in COVID-19.
The researchers also used mouse models to confirm that autoantibodies from patients with COVID-19 actually led to blood clots. Again, those findings closely mirror what happens in mouse studies testing the effects of antibodies from patients with the most severe forms of antiphospholipid syndrome.
While more study is needed, the findings suggest that treatments directed at autoantibodies to limit the formation of NETs might improve outcomes for people severely ill with COVID-19. The researchers note that further study is needed to determine what triggers autoantibodies in the first place and how long they last in those who’ve recovered from COVID-19.
The researchers have already begun enrolling patients into a modest scale clinical trial to test the anti-clotting drug dipyridamole in patients who are hospitalized with COVID-19, to find out if it can protect against dangerous blood clots. These observations may also influence the design of the ACTIV-4 trial, which is testing various antithrombotic agents in outpatients, inpatients, and convalescent patients. Kanthi and Knight suggest it may also prove useful to test infected patients for aPL antibodies to help identify and improve treatment for those who may be at especially high risk for developing clots. The hope is this line of inquiry ultimately will lead to new approaches for avoiding this very troubling complication in patients with severe COVID-19.
Reference:
[1] Prothrombotic autoantibodies in serum from patients hospitalized with COVID-19. Zuo Y, Estes SK, Ali RA, Gandhi AA, Yalavarthi S, Shi H, Sule G, Gockman K, Madison JA, Zuo M, Yadav V, Wang J, Woodard W, Lezak SP, Lugogo NL, Smith SA, Morrissey JH, Kanthi Y, Knight JS. Sci Transl Med. 2020 Nov 2:eabd3876.
Links:
Coronavirus (COVID-19) (NIH)
Antiphospholipid Antibody Syndrome (National Heart Lung and Blood Institute/NIH)
Kanthi Lab (National Heart, Lung, and Blood Institute, Bethesda, MD)
Knight Lab (University of Michigan)
ACTIV (NIH)
NIH Support: National Heart, Lung, and Blood Institute

Very nice explanation. Thank you for sharing such valuable article.
Thin blood and prescribe steroids
Elevated ANA without symptoms can most often be explained by close urban living and the exposure to foreign human and animal nuclear material.
I had a real blog success because of your lovely material. You’re fantastic. You’re great. It’s an interesting blog.
Could this autoimmune response occur with vaccine? Can some people with autoimmune disorder develop these antibodies when the vaccines developed by Moderna and Pfizer are given?
I too am curious to know about the same thing. With the vaccine, my hope is that it would not lead to the amount of blood clots in the way the virus would, since the virus grows in the body, whereas the spike protein in the vaccine would not. But definitely there will be some kind of auto immune response which could lead to blood clots, though not as severe as the virus. But the question is, can someone risk it knowing they could end up in the hospital? Doctors are not willing to say much about this, they say they do not have data.
My 85 y/o mom got the COVID 19 vaccine last week and 5 days later she developed a DVT that progressed to PE 2 days after that. She has never had a blood clot before and has no other known risk factors other than age. Should she get the second dose?
I’m 50 years old and had a left arm DVT as well (same arm as the vaccine). Luckily, the CT scan I had done didn’t show a PE at this time. I decided to skip the second dose for now. I got Moderna. Which one did your mom get?
Hi! I’m 51 y/o with no medical problems and no history of clots. I got my first dose of the Pfizer vaccine on Dec 27th and was hospitalized with an unprovoked acute pulmonary embolism on January 13th. My concern for this being a possible inappropriate inflammatory response to the vaccine has fallen on deaf ears. I hope the the proper officials look into this before someone dies.
My best friend is an active 39 years old with no medical problems and no history of clots. She got her first dose of the Pfizer vaccine on 1st February 2021, and was hospitalized with an unprovoked acute pulmonary embolism on 13th February 2021. Coincidence much?! She’s currently in hospital having anticoagulant injections in her stomach and is having a scan on her heart tomorrow because the doctors say the clot is so large in her lung, as well as there being several smaller clots developing rapidly, that it’s putting too much pressure on her heart. I’m terrified, and I can’t help but think that this is as a result of the vaccine.
Oh my goodness! I hope she gets better soon! It’s a very scary experience and I hope someone of authority will address the problem before someone dies.
Question for Tinkerbell and Stephanie: how did things go after your last posts? Recovered? Still issues? Asking because we have a PE case (in close family) which showed first symptoms around 3 days after 1st dose of Pfizer. A few days later, it required several days in hospital and led to anticoagulant prescription for several months. The family member has no history of clots, has a normal weight and average fitness level.
Did you get a clotting factor to see why the clot happened? It could be a genetic trait?
I am a 47 y.o. first responder. I received the Moderna vaccine on Jan 25, 2021. I was diagnosed with one large and several smaller P.E.’s on February 8, 2021, and was prescribed anticoagulants for three months. I have had no history of blood clotting, nor is there any family history. I am in reasonably good shape with no health issues. Currently, the thought was that I had developed the P.E.’s due to a 6-hour car trip that I’ve made on occasion before with zero issues. Since then, I’ve received my 2nd Moderna shot on Feb. 22, and have not had any additional issues. I have been searching to find any articles regarding the possibility of clotting as a side effect, but have not found anything until this blog. It may just be a coincidence, although, it sounds as there are more out there than just myself with this concern.
I also went through an emergency room for P.E due to a clot in my lungs from confirmed came from my right thigh. This incident happened on Jan 15, 2021. I was tested for Covid 19 negative. I never test for covid 19 until that day. I believe i never had any major symptom of covid like fever except my allergy symptom. Prior to that i had no history as wells as no family history at all. Also, i am 51 year of age and i don’t have any diseases except for seasonal allergy. I have received my Moderna vaccine both shots in february and March 2021. I am also on pradaxa blood thinner since Jan 15. Doctor could not find any reason and done number of test but not a clue why this happened. Doctor mentioned that i may have to be on pradaxa for life, which gives me a nervous break down. Now i am started to believe that what if i had very light covid symptom with NO fever and did not know about it, which may have caused blood clot from covid. But now i cannot go back to find out. My first Lupus anticoagulant test came positive and second time it came back negative.
I am also a first responder who had the Moderna vaccine (second does Feb 2nd). Made a trip to the ER last night with a back injury and some thoracic discomfort. They decided to give me a full workup. D-dimer was 2.6 (normal is less than 0.6). They immediately sent me for a CT Angiogram and found that I had two right sided PE’s that were small enough not to cause symptoms but also some recent infarcts in my lungs. Never had any clotting issues or history in my family. I was like you Dan looking for information about any correlation between the vaccine and PE’s and your post on this blog is what I found. I asked the ER Doc about this and she said it is very possible that this could have been a side effect of the vaccine. My case was mild and I was sent home from the ER with Xarelta and asked to follow up with my physician. Keeping hearing about cases like this but nobody in the mainstream will talk about it. Makes me nervous when they keep shutting down open discussions about Covid vaccines. I keep reminding people that this vaccine has “Emergency” approval and anyone who states that this vaccine is 100% safe “long term” is either not being honest or un-informed. The reality is that this vaccine could have have side effects we don’t know about yet. I still obviously felt the decision to get vaccinated was the right decision for me and my family. I just want everyone to have all the information so they can make the right decision for them. Thanks for your post Dan K.
Has anyone considered the Vaccine AstraZeneca which has been suspended in many countries due to blood clotting may have too much traces of COVID-19 in it?
Hi I am a 60 y.o. writer with Systemic Sclerosis. I had the first shot of AstroZeneca on Friday 5 February and was rushed to hospital on Friday 12 January with a clot on the brain. I’m recovering but it has left me impaired.
What I find particularly frustrating is that I asked about vaccine side effects in a video call with a renowned medical institution in late January and was told to go ahead and have the vaccine, there would be no problems. Now I see you were raising concerns about the side effects, especially for people with rheumatic conditions, before Christmas.
I know we need to vaccinate everyone and scare stories have to be played down but you’d think the UK’s top Sclero unit would know about the possibility of clots and frankly, I would like to have been made aware of the risk.
What if you have no T cells,antiphosolipid and lupus? Can you receive the vaccine safety ?
I was scheduled to get pfizer and googled COVID vac and antiphophlipid antibody syndrome (APS). Did not get shot after reading these posts. I think best to wait until “DATA” comes in. Maybe people with APS should have heparin and steriods before getting vac and stay on for a while afterwards. Or, maybe J&J would be safer. I had 6 miscarriages and that’s how I found out I have this syndrome. Had I never gotten prego I probably would not have known I had it. Hope the powers that be look into this.
My husbands INR dropped to 1.3 about 3 weeks after Moderna vaccine and his therapeutic range is 2.5-3.5. We don’t think he missed a dose of his Coumadin and by reading about these instances of blood clots after receiving the vaccine convinces me this is attributed to the vaccine. I’m very concerned because he had a mechanical mitral valve put in about 4 months ago. And he took his second vaccine shot the day before his inr lab draw so I’m even more concerned it may continue to be sub therapeutic. We are going to has his level redrawn in a few days and maybe continue twice a week for a couple weeks. We can’t be 100% sure he didn’t miss a dose but it doesn’t seem likely.
Can I receive a covid vaccine if during my last pregnancy I tested positive in APAS ( Antiphospholipid Antibody Syndrome)? I’m afraid it will trigger may APAS if i get vaccinated.
May 2020 I had what I thought was a seizure/blackout and ended up in the ER. Nothing showed up on the CT scan or MRI. Referred me to a cardiologist who gave me every test and scan possible, no signs of blockages, leaky heart, irregular heart beat, said I must have fainted and sent me on my way. A month later I had a TIA and ended up in the ER again. Once again, they could find no reason why I would have a TIA. Sent me to a neurologist. Blood tests indicated antiphospholipid antibodies. Told me I probably had APS and put me on blood thinners and baby aspirin. Repeated the tests after 3 months, still positive so they confirmed I had APS and referred me to a hematologist. Had blood tests again to determine what the correct amount of Warfarin I should take…got a call a week later saying all of my blood tests came back normal. I think I had asymptomatic covid in March 2020, and these events were the result. Can’t get any confirmation from anyone though.
It would be very interesting to investigate if these autoantibodies are involved in Long Covid and ME/CFS. There may be an undiscovered autoimmune aspect to these illnesses.
I have had ME/CFS for 23 years and in addition I developed an unexplained thrombocytopenia. I had a positive ANA test, for what it’s worth, on multiple occasions. No one understands the mechanism behind all of this. I reacted positively to IVIg treatment, but unfortunately it had to be stopped because of regulatory reasons.