Insights into Molecular Basis of PTSD and Major Depression Could One Day Aid in Diagnosis and Treatment
Posted on by Dr. Monica M. Bertagnolli
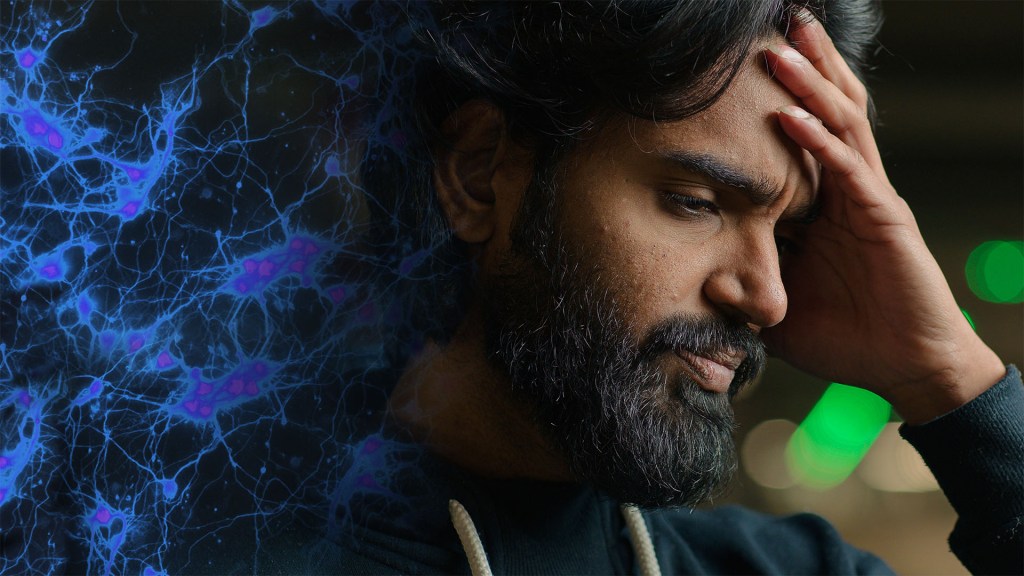
We know stress can take a toll on our mental health. Yet, it’s unclear why some people develop stress-related mental health disorders and others don’t. The risk for developing a stress-related mental health disorder such as post-traumatic stress disorder (PTSD) or major depressive disorder (MDD) depends on a complex interplay between the genetic vulnerabilities we are born with and the impact of traumatic stress we experience over our lifetimes.
Given this complexity, it’s been difficult for researchers to pinpoint the underlying biological pathways in the body that ultimately produce changes associated with PTSD, major depression, or other mental health conditions. Now, a study reported in a special issue of Science on decoding the brain uses a comprehensive approach to examine multiple biological processes across brain regions, cell types, and blood to elucidate this complexity. It’s an unprecedented effort to understand in a more holistic way the essential biological networks involved in PTSD and MDD.
While earlier studies looked at stress hormones, the immune system, and other molecular signatures of stress in blood samples, what had been largely missing from the picture of PTSD and MDD were links between those changes in the body and changes in the brain. To get a more complete picture, a multisite research team led by Nikolaos P. Daskalakis and Kerry Ressler of McLean Hospital, Belmont, MA, developed a vast molecular dataset including DNA variants, RNA, proteins, and chemical modifications to DNA. This “multi-omic” dataset was generated by the NIH-supported PTSD Brainomics Project of the PsychENCODE Consortium, and included postmortem data from 231 individuals with PTSD and/or MDD, as well as from individuals who didn’t have known mental health conditions.
In the study, the researchers looked at three essential brain regions: the medial prefrontal cortex (mPFC), the hippocampal dentate gyrus, and the central nucleus of the amygdala. They conducted single-cell RNA sequencing analysis of 118 dorsolateral prefrontal cortex (dlPFC) samples to look at cell-type-specific patterns and evaluated protein changes in the blood of more than 50,000 UK Biobank samples to look for biomarkers of stress-related disorders. After identifying key brain-based genes whose expression was altered in PTSD and/or MDD, the researchers compared them to genes linked to increased risk for these conditions.
Among many findings, the study results show an important role for the mPFC in both stress-related conditions, which is interesting, as the mPFC is essential for integrating signals from other brain areas and is known to play a role in cognitive processes, emotional regulation, motivation, and sociability. The findings also highlight important roles for molecular pathways known to play a role in immune function, the regulation of neurons and neural connections, and stress hormones. The single-cell RNA sequencing in the dlPFC also uncovered dysregulated stress-related signals in neurons and other brain cell types.
Furthermore, the findings reveal shared changes in gene activity between PTSD and MDD, as well as notable differences in the patterns of methyl marks on the DNA, suggesting changes in the way genes are switched on or off, and at the level of cell-type-specific gene activity. The researchers also found that history of childhood trauma and suicide were drivers of molecular changes in both disorders.
The data point to a short list of proteins that may be important in regulating key genetic pathways underlying these disorders. They also reveal links to gene networks related to aging, inflammation, stress, and more. Similarities in disease signals in the brain and blood suggest that blood-based tests might one day offer an additional avenue for assessing these disorders. Interestingly, there was little overlap between PTSD and MDD risk genes and those involved in the underlying molecular-level changes in the brains of people with one or both conditions. This shows that there’s a need for more research into how genetic risk factors are related to molecular-level disease processes.
There’s clearly much more to discover in the years ahead. But these insights already point to important roles for known stress-related pathways in fundamental brain changes underlying PTSD and MDD, while also revealing more novel pathways as potentially promising new treatment targets. With further study, the researchers hope these findings can also begin to answer vexing questions, such as why some people develop PTSD or major depression after stressful events and others don’t.
Reference:
Daskalakis NP, et al. Systems biology dissection of PTSD and MDD across brain regions, cell types, and blood. Science. DOI: 10.1126/science.adh3707 (2024).
This paper is part of a larger collection of studies from the PsychENCODE Consortium looking at the underlying mechanisms of neuropsychiatric diseases.
NIH Support: National Institute of Mental Health

After the suicide of our younger teenage sister, my older sister and I both ended up with MDD later in life. I have also been diagnosed 20 years ago with PTSD also due to my career. We both have had multiple hospitalizations because of suicidal ideation. My sister and I continue to be medicated with antidepressants/ neuroleptics. My sister is 72 and I soon will see my 70th birthday. We both are grateful for life and feel that the severity of symptoms have diminished with age. We have both spent many years in cognitive behavioral therapy which has given us insight into our family background in development, both physical and mental. Thank you for this article that has asserted the ailments may indeed have a genetic component that might someday be identified and treated. Good wishes for continued research.