For many people struggling with depression, antidepressants and talk therapy can help to provide relief. But for some, the treatments don’t help nearly enough. I’m happy to share some early groundbreaking research in alleviating treatment-resistant depression in a whole new way: implanting a pacemaker-like device capable of delivering therapeutic electrical impulses deep into the brain, aiming for the spot where they can reset the depression circuit.
What’s so groundbreaking about the latest approach—so far, performed in just one patient—is that the electrodes didn’t simply deliver constant electrical stimulation. The system could recognize the specific pattern of brain activity associated with the patient’s depressive symptoms and deliver electrical impulses to the brain circuit where it could provide the most relief.
While much more study is needed, this precision approach to deep brain stimulation (DBS) therapy offered immediate improvement to the patient, a 36-year-old woman who’d suffered from treatment-resistant major depressive disorder since childhood. Her improvement has lasted now for more than a year.
This precision approach to DBS has its origins in clinical research supported through NIH’s Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative. A team, led by Edward Chang, a neurosurgeon at the University of California San Francisco’s (UCSF) Epilepsy Center, discovered while performing DBS that the low mood in some patients with epilepsy before surgery was associated with stronger activity in a “subnetwork” deep within the brain’s neural circuitry. The subnetwork involved crosstalk between the brain’s amygdala, which mediates fear and other emotions, and the hippocampus, which aids in memory.
Researchers led by Andrew Krystal, UCSF, Weill Institute for Neurosciences, attempted in the latest work to translate this valuable lead into improved care for depression. Their results were published recently in the journal Nature Medicine [1].
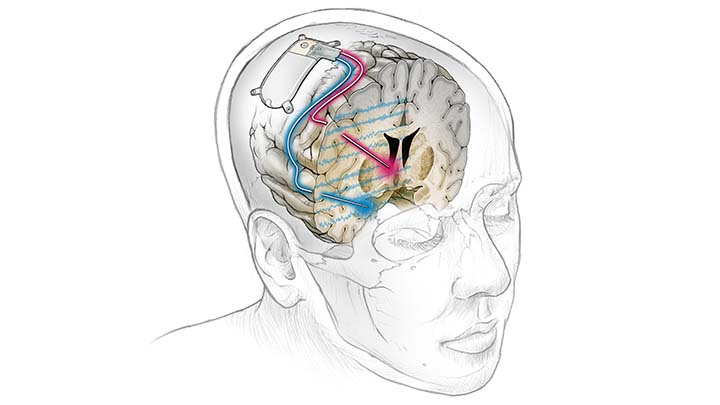
Krystal and colleagues, including Chang and Katherine Scangos, who is the first author of the new study, began by mapping patterns of brain activity in the patient that was associated with the onset of her low moods. They then customized an FDA-approved DBS device to respond only when it recognized those specific patterns. Called NeuroPace® RNS®, the device includes a small neurostimulator and measures about 6 by 3 centimeters, allowing it to be fully implanted inside a person’s skull. There, it continuously monitors brain activity and can deliver electrical stimulation via two leads, as shown in the image above [2].
Researchers found they could detect and predict high symptom severity best in the amygdala, as previously reported. The next question was where the electrical stimulation would best relieve those troubling brain patterns and associated symptoms. They discovered that stimulation in the brain’s ventral capsule/ventral striatum, part of the brain’s circuitry for decision-making and reward-related behavior, led to the most consistent and sustained improvements. Based on these findings, the team devised an on-demand and immediate DBS therapy that was unique to the patient’s condition.
It will be important to learn whether this precision approach to DBS is broadly effective for managing treatment-resistant depression and perhaps other psychiatric conditions. It will take much more study and time before such an approach to treating depression can become more widely available. Also, it is not yet clear just how much it would cost. But these remarkable new findings certainly point the way toward a promising new approach that will hopefully one day bring another treatment option for those in need of relief from severe depression.
References:
[1] Closed-loop neuromodulation in an individual with treatment-resistant depression. Scangos KW, Khambhati AN, Daly PM, Makhoul GS, Sugrue LP, Zamanian H, Liu TX, Rao VR, Sellers KK, Dawes HE, Starr PA, Krystal AD, Chang EF. Nat Med. 2021 Oct;27(10):1696-1700
[2] The NeuroPace® RNS® System for responsive neurostimulation, NIH BRAIN Initiative.
Links:
Depression (National Institute of Mental Health/NIH)
Deep Brain Stimulation for Parkinson’s Disease and other Movement Disorders (National Institute of Neurological Disorders and Stroke/NIH)
Andrew Krystal (University of California San Francisco)
Katherine Scangos (UCSF)
Edward Chang (UCSF)
NIH Support: National Institute of Neurological Disorders and Stroke