ACTIV-4
Can Blood Thinners Keep Moderately Ill COVID-19 Patients Out of the ICU?
Posted on by Dr. Francis Collins
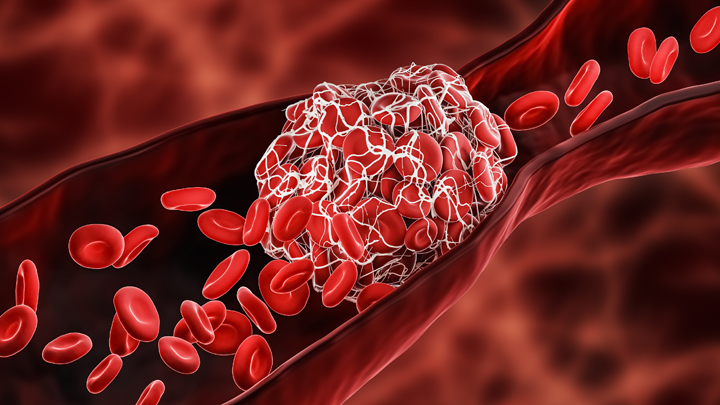
One of many troubling complications of infection with SARS-CoV-2, the coronavirus that causes COVID-19, is its ability to trigger the formation of multiple blood clots, most often in older people but sometimes in younger ones, too. It raises the question of whether and when more aggressive blood thinning treatments might improve outcomes for people hospitalized for COVID-19.
The answer to this question is desperately needed to help guide clinical practice. So, I’m happy to report interim results of three large clinical trials spanning four continents and more than 300 hospitals that are beginning to provide critical evidence on this very question [1]. While it will take time to reach a solid consensus, the findings based on more than 1,000 moderately ill patients suggest that full doses of blood thinners are safe and can help to keep folks hospitalized with COVID-19 from becoming more severely ill and requiring some form of organ support.
The results that are in so far suggest that individuals hospitalized, but not severely ill, with COVID-19 who received a full intravenous dose of the common blood thinner heparin were less likely to need vital organ support, including mechanical ventilation, compared to those who received the lower “prophylactic” subcutaneous dose. It’s important to note that these findings are in contrast to results announced last month indicating that routine use of a full dose of blood thinner for patients already critically ill and in the ICU wasn’t beneficial and may even have been harmful in some cases [2]. This is a compelling example of how critical it is to stratify patients with different severity in clinical trials—what might help one subgroup might be of no benefit, or even harmful, in another.
More study is clearly needed to sort out all the details about when more aggressive blood thinning treatment is warranted. Trial investigators are now working to make the full results available to help inform a doctor’s decisions about how to best to treat their patients hospitalized with COVID-19. It’s worth noting that these trials are overseen by independent review boards, which routinely evaluate the data and are composed of experts in ethics, biostatistics, clinical trials, and blood clotting disorders.
These clinical trials were made possible in part by the Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) public-private partnership and its ACTIV-4 Antithrombotics trials—along with similar initiatives in Canada, Australia, and the European Union. The ACTIV-4 trials are overseen by the NIH’s National Heart, Lung, and Blood institute and funded by Operation Warp Speed.
This ACTIV-4 trial is one of three Phase 3 clinical trials evaluating the safety and effectiveness of blood thinners for patients with COVID-19 [3]. Another ongoing trial is investigating whether blood thinners are beneficial for newly diagnosed COVID-19 patients who do not require hospitalization. There are also plans to explore the use of blood thinners for patients after they’ve been discharged from the hospital following a diagnosis of moderate to severe COVID-19 and to establish more precise methods for identifying which patients with COVID-19 are most at risk for developing life-threatening blood clots.
Meanwhile, research teams are exploring other potentially promising ways to repurpose existing therapeutics and improve COVID-19 outcomes. In fact, the very day that these latest findings on blood thinners were announced, another group at The Montreal Heart Institute, Canada, announced preliminary results of the international COLCORONA trial, testing the use of colchicine—an anti-inflammatory drug widely used to treat gout and other conditions—for patients diagnosed with COVID-19 [4].
Their early findings in treating patients just after a confirmed diagnosis of COVID-19 suggest that colchicine might reduce the risk of death or hospitalization compared to patients given a placebo. In the more than 4,100 individuals with a proven diagnosis of COVID-19, colchicine significantly reduced hospitalizations by 25 percent, the need for mechanical ventilation by 50 percent, and deaths by 44 percent. Still, the actual numbers of individuals represented by these percentages was small.
Time will tell whether and for which patients colchicine and blood thinners prove most useful in treating COVID-19. For those answers, we’ll have to await the analysis of more data. But the early findings on both treatment strategies come as a welcome reminder that we continue to make progress each day on such critical questions about which existing treatments can be put to work to improve outcomes for people with COVID-19. Together with our efforts to slow the spread of SARS-CoV-2, finding better ways to treat those who do get sick and prevent some of the worst outcomes will help us finally put this terrible pandemic behind us.
References:
[1] Full-dose blood thinners decreased need for life support and improved outcome in hospitalized COVID-19 patients. National Heart, Lung, and Blood Institute. January 22, 2021.
[2] NIH ACTIV trial of blood thinners pauses enrollment of critically ill COVID-19 patients. National Heart, Lung, and Blood Institute. December 22, 2020.
[3] NIH ACTIV initiative launches adaptive clinical trials of blood-clotting treatments for COVID-19. National Heart, Lung, and Blood Institute. September 10, 2020.
[4] Colchicine reduces the risk of COVID-19-related complications. The Montreal Heart Institute. January 22, 2021.
Links:
COVID-19 Research (NIH)
Combat COVID (U.S. Department of Health and Human Services, Washington, D.C.)
Accelerating COVID-19 Therapeutic Interventions and Vaccines (ACTIV) (NIH)
NIH Support: National Heart, Lung, and Blood Institute
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)
Posted In: News
Tags: Accelerating COVID-19 Therapeutic Interventions and Vaccines, ACTIV, ACTIV-4, ACTIV-4 Antithrombotics trials, blood, blood clots, blood thinner, blood vessels, clinical trials, colchicine, COLCORONA trial, COVID-19, COVID-19 treatment, COVID-19-complications, heart, heparin, Montreal Heart Institute, novel coronavirus, pandemic, SARS-CoV-2, stroke
