3D printing
Snapping Together a New Microlab
Posted on by Dr. Francis Collins
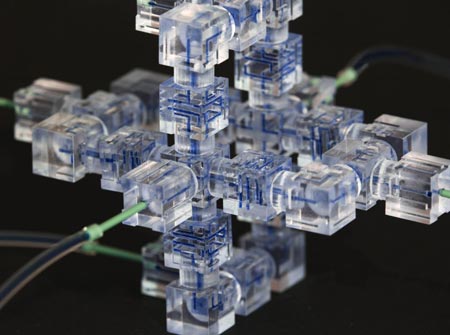
Just as the computational power of yesterday’s desktop computer has been miniaturized to fit inside your mobile phone, bioengineers have shrunk traditional laboratory instruments to the size of a dime. To assemble a “snap lab” like the one you see above, all scientists have to do is click together some plastic components in much the same way that kids snap together the plastic bricks in their toy building sets.
The snap lab, developed by an NIH-funded team led by Noah Malmstadt at the University of Southern California (USC) Viterbi School of Engineering, Los Angeles, is an exciting example of a microfluidic circuit—tiny devices designed to test just a single drop of blood, saliva, or other fluids. Such devices have the potential to make DNA analysis, microbe detection, and other biomedical tests easier and cheaper to perform.
Previous Page