32 Search Results for "Prescription"
Bringing Out the Best in Us During the Pandemic
Posted on by Dr. Francis Collins

Sheltering at home for more than two months has made many of us acutely aware of just how much we miss getting out and interacting with other human beings. For some, the coronavirus disease 2019 (COVID-19) pandemic has also triggered a more selfless need: to be a good neighbor to the most vulnerable among us and help them stay well, both mentally and physically, during this trying time.
The term “good neighbor” definitely applies to Pablo Vidal-Ribas Belil, a postdoctoral fellow at NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). Though Vidal-Ribas has his hands full caring for his 4-year-old son in their condo, which is located near NIH’s main campus in Bethesda, MD, he wasn’t too busy to notice that some of his neighbors were in need of help.
Vidal-Ribas extended a helping hand to pick up groceries and prescriptions for the older woman downstairs, as well as several more of his elderly neighbors. He and other concerned neighbors also began enlisting more volunteers to join a neighborhood coronavirus task force. There are now up to 30 volunteers and sometimes hold virtual meetings.
To try to reach everyone in the more than 950-unit Parkside Condominium community, the group coordinated its activities with the help of the management office. They also issued flyers and email messages via the neighborhood list serv, offering to assist people at greatest risk for COVID-19, including seniors and those with compromised immune systems or other serious conditions, by shopping for essential items and dropping the items off at their doors.
The personal interest and care of Vidal-Ribas also comes with medical expertise: he’s a clinical psychologist by training. Vidal-Ribas, who is originally from Barcelona, Spain, came to the United States four years ago to work with an NIH lab that specializes in the study of depression and related conditions in young people. Last year, Vidal-Ribas moved to NICHD as a Social and Behavioral Sciences Branch Fellow, where he now works with Stephen Gilman. There, he explores prenatal and early developmental factors that contribute to attempts at suicide later in life.
His expertise as a psychologist has come in handy. Vidal-Ribas has found that many of the individuals requesting help with grocery items or prescriptions also want to talk. So, the team’s efforts go a long way toward providing not only basic necessities, but also much-needed social and emotional support.
In recognition of this need, the group has expanded to offer virtual chats and other community activities, such as physically distanced games, conversations, or story times. One talented young volunteer has even offered to give music concerts remotely by request. Folks know they can call on Vidal-Ribas and some of the most active task force volunteers at any time.
Vidal-Ribas reports that they’ve taken great care to follow the latest guidelines from the Centers for Disease Control and Prevention on how to protect yourself and others from COVID-19 to ensure that those volunteering their time do so safely. He and other volunteers typically buy for multiple neighbors at once while they do their own personal shopping to reduce the number of outings. They then leave the bags with groceries or prescriptions at their neighbors’ doors with no direct contact. As far as he knows, none of his vulnerable neighbors have come down with COVID-19.
Vidal-Ribas says he’s prepared to continue his volunteer outreach for as long as it takes. And, even when the threat of COVID-19 subsides, he’ll keep on lending a hand to his neighbors. It’s one of the ways he stays connected to his community and grounded within himself during this difficult time. By sharing his story, he hopes it will inspire others to do what they can to help others in need to stay safe and well.
Links:
Coronavirus (COVID-19) (NIH)
Social and Behavioral Sciences Branch Fellows (National Institute of Child Health and Human Development/NIH)
Stephen Gilman ((National Institute of Child Health and Human Development/NIH)
After Opioid Overdose, Most Young People Aren’t Getting Addiction Treatment
Posted on by Dr. Francis Collins

Drug overdoses continue to take far too many lives, driven primarily by the opioid crisis (though other drugs, such as methamphetamine and cocaine, are also major concerns). While NIH’s Helping to End Addiction Long-term (HEAL) Initiative is taking steps to address this terrible crisis, new findings serve as another wake-up call that young people battling opioid addiction need a lot more assistance to get back on the right track.
In a study of more than 3,600 individuals, aged 13-22, who survived an opioid overdose, an NIH-funded team found that only about one-third received any kind of follow-up addiction treatment [1]. Even more troubling, less than 2 percent of these young people received the gold standard approach of medication treatment.
The findings reported in JAMA Pediatrics come from Rachel Alinsky, an adolescent medicine and addiction medicine fellow at Johns Hopkins Children’s Center, Baltimore. She saw first-hand the devastating toll that opioids are taking on our youth.
Alinsky also knew that nationally more than 4,000 fatal opioid overdoses occurred in people between the ages of 15 and 24 in 2016 [2]. Likewise, rates of nonfatal opioid overdoses for teens and young adults also have been escalating, leading to more than 7,000 hospitalizations and about 28,000 emergency department visits in 2015 alone [3].
In the latest study, Alinsky wanted to find out whether young people who overdose receive timely treatment to help prevent another life-threatening emergency. According to our best evidence-based guidelines, timely treatment for youth with an opioid addiction should include medication, ideally along with behavioral interventions.
That’s because opioid addiction rewires the brain—will power alone is simply not sufficient to achieve and sustain recovery. After one overdose, the risk of dying from another one rises dramatically. So, it is critical to get those who survived an overdose into effective treatment right away.
Alinsky and her team dove into the best-available dataset, consisting of data on more than 4 million mostly low-income adolescents and young adults who’d been enrolled in Medicaid for at least six months in 16 states. The sample included 3,606 individuals who’d been seen by a doctor and diagnosed with opioid poisoning. A little over half of them were female; most were non-Hispanic whites.
Heroin accounted for about a quarter of those overdoses. The rest involved other opioids, most often prescription painkillers. However, the researchers note that some overdoses attributed to heroin might have been caused by the powerful synthetic opioid fentanyl. The use of fentanyl, often mixed with heroin, was on the rise in the study’s final years, but it was rarely included in drug tests at the time.
Less than 20 percent of young people in the sample received a diagnosis of opioid use disorder, or a problematic pattern of opioid use resulting in impairment or distress. What’s more, in the month following an overdose, few received the current standard for addiction treatment, which should include behavioral therapy and treatment with one of three drugs: buprenorphine, naltrexone, or methadone.
Drilling a little deeper into the study’s findings:
• 68.9 percent did not receive addiction treatment of any kind.
• 29.3 percent received behavioral health services alone.
• Only 1.9 percent received one of three approved medications for opioid use disorder.
It’s been estimated previously that teens and young adults are one-tenth as likely as adults 25 years and older to get the recommended treatment for opioid use disorder [4]. How can that be? The researchers suggest that one factor might be inexperience among pediatricians in diagnosing and treating opioid addiction. They also note that, even when the problem is recognized, doctors sometimes struggle to take the next step and connect young people with addiction treatment facilities that are equipped to provide the needed treatment to adolescents.
As this new study shows, interventions designed to link teens and young adults with the needed recovery treatment and care are desperately needed. As we continue to move forward in tackling this terrible crisis through the NIH’s HEAL Initiative and other efforts, finding ways to overcome such systemic barriers and best engage our youth in treatment, including medication, will be essential.
References:
[1] Receipt of addiction treatment after opioid overdose among Medicaid-enrolled adolescents and young adults. Alinsky RH, Zima BT, Rodean J, Matson PA, Larochelle MR, Adger H Jr, Bagley SM, Hadland SE. JAMA Pediatr. 2020 Jan 6:e195183.
[2] Overdose death rates. National Institute on Drug Abuse, NIH.
[3] 2018 annual surveillance drug-related risks and outcomes—United States: surveillance special report. Centers for Disease Control and Prevention.
[4] Medication-assisted treatment for adolescents in specialty treatment for opioid use disorder. Feder KA, Krawczyk N, Saloner B. J Adolesc Health. 2017 Jun;60(6):747-750.
Links:
Opioid Overdose Crisis (National Institute on Drug Abuse/NIH)
Opioid Overdose (Centers for Disease Control and Prevention, Atlanta)
Decisions in Recovery: Treatment for Opioid Use Disorder (Substance Abuse and Mental Health Services Administration, Rockville, MD)
Rachel Alinsky (Johns Hopkins University Children’s Center, Baltimore)
Helping to End Addiction Long-term (HEAL) Initiative (NIH)
NIH Support: Eunice Kennedy Shriver National Institute of Child Health and Human Development; National Institute on Drug Abuse
Panel Finds Exercise May Lower Cancer Risk, Improve Outcomes
Posted on by Dr. Francis Collins

Exercise can work wonders for your health, including strengthening muscles and bones, and boosting metabolism, mood, and memory skills. Now comes word that staying active may also help to lower your odds of developing cancer.
After reviewing the scientific evidence, a panel of experts recently concluded that physical activity is associated with reduced risks for seven common types of cancer: colon, breast, kidney, endometrial, bladder, stomach, and esophageal adenocarcinoma. What’s more, the experts found that exercise—both before and after a cancer diagnosis—was linked to improved survival among people with breast, colorectal, or prostate cancers.
About a decade ago, the American College of Sports Medicine (ACSM) convened its first panel of experts to review the evidence on the role of exercise in cancer. At the time, there was limited evidence to suggest a connection between exercise and a reduced risk for breast, colon, and perhaps a few other cancer types. There also were some hints that exercise might help to improve survival among people with a diagnosis of cancer.
Today, the evidence linking exercise and cancer has grown considerably. That’s why the ACSM last year convened a group of 40 experts to perform a comprehensive review of the research literature and summarize the level of the evidence. The team, including Charles Matthews and Frank Perna with the NIH’s National Cancer Institute, reported its findings and associated guidelines and recommendations in three papers just published in Medicine & Science in Sports & Exercise and CA: A Cancer Journal for Clinicians [1,2,3].
Here are some additional highlights from the papers:
There’s moderate evidence to support an association between exercise and reduced risk for some other cancer types, including cancers of the lung and liver.
While the optimal amount of exercise needed to reduce cancer risk is still unclear, being physically active is clearly one of the most important steps in general that people of all ages and abilities can take.
Is sitting the new smoking? Reducing the amount of time spent sitting also may help to lower the risk of some cancers, including endometrial, colon, and lung cancers. However, there’s not enough evidence to draw clear conclusions yet.
Every cancer survivor should, within reason, “avoid inactivity.” There’s plenty of evidence to show that aerobic and resistance exercise training improves many cancer-related health outcomes, reducing anxiety, depression, and fatigue while improving physical functioning and quality of life.
Physical activity before and after a diagnosis of cancer also may help to improve survival in some cancers, with perhaps the greatest benefits coming from exercise during and/or after cancer treatment.
Based on the evidence, the panel recommends that cancer survivors engage in moderate-intensity exercise, including aerobic and resistance training, at least two to three times a week. They should exercise for about 30 minutes per session.
The recommendation is based on added confirmation that exercise is generally safe for cancer survivors. The data indicate exercise can lead to improvements in anxiety, depression, fatigue, overall quality of life, and in some cases survival.
The panel also recommends that treatment teams and fitness professionals more systematically incorporate “exercise prescriptions” into cancer care. They should develop the resources to design exercise prescriptions that deliver the right amount of exercise to meet the specific needs, preferences, and abilities of people with cancer.
The ACSM has launched the “Moving Through Cancer” initiative. This initiative will help raise awareness about the importance of exercise during cancer treatment and help support doctors in advising their patients on those benefits.
It’s worth noting that there are still many fascinating questions to explore. While exercise is known to support better health in a variety of ways, correlation is not the same as causation. Questions remain about the underlying mechanisms that may help to explain the observed associations between physical activity, lowered cancer risk, and improved cancer survival.
An intensive NIH research effort, called the Molecular Transducers of Physical Activity Consortium (MoTrPAC), is underway to identify molecular mechanisms that might explain the wide-ranging benefits of physical exercise. It might well shed light on cancer, too.
As that evidence continues to come in, the findings are yet another reminder of the importance of exercise to our health. Everybody—people who are healthy, those with cancer, and cancer survivors alike—should make an extra effort to remain as physically active as our ages, abilities, and current health will allow. If I needed any more motivation to keep up my program of vigorous exercise twice a week, guided by an experienced trainer, here it is!
References:
[1] Exercise Is Medicine in Oncology: Engaging Clinicians to Help Patients Move Through Cancer. Schmitz KH, Campbell AM, Stuiver MM, Pinto BM, Schwartz AL, Morris GS, Ligibel JA, Cheville A, Galvão, DA, Alfano CM, Patel AV, Hue T, Gerber LH, Sallis R, Gusani NJ, Stout NL, Chan L, Flowers F, Doyle C, Helmrich S, Bain W, Sokolof J, Winters-Stone KM, Campbell KL, Matthews CE. CA Cancer J Clin. 2019 Oct 16 [Epub ahead of publication]
[2] American College of Sports Medicine Roundtable Report on Physical Activity, Sedentary Behavior, and Cancer Prevention and Control. Patel AV, Friedenreich CM, Moore SC, Hayes SC, Silver JK, Campbell KL, Gerber LH, George SM, Fulton JE, Denlinger C, Morris GS, Hue T, Schmitz KH, Matthews CE. Med Sci Sports Exerc. 2019 Oct 16. [Epub ahead of publication]
[3] Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Campbell KL, Winters-Stone KM, Wiskemann J, May AM, Schwartz AL, Courneya KS, Zucker DS, Matthews CE, Ligibel JA, Gerber LH, Morris GS, Patel AV, Hue TF, Perna FM, Schmitz KH. Med Sci Sports Exerc. 2019 Oct 16. [Epub ahead of publication]
Links:
Physical Activity and Cancer (National Cancer Institute/NIH)
Moving Through Cancer (American College of Sports Medicine, Indianapolis, IN)
American College of Sports Medicine
Charles Matthews (NCI)
Frank Perna (NCI)
NIH Support: National Cancer Institute
Easier Access to Naloxone Linked to Fewer Opioid Deaths
Posted on by Dr. Francis Collins

A few weeks ago, I was pleased to take part in the announcement of NIH’s HEALing Communities Study in four states hard hit by the opioid epidemic. This study will test a comprehensive, evidence-based approach—which includes the wide distribution of naloxone to reverse overdoses—with the aim of reducing opioid-related deaths in selected communities by 40 percent over three years.
That’s a very ambitious goal. So, I was encouraged to read about new findings that indicate such reductions may be within our reach if society implements a number of key changes. Among those is the need to arm friends, family members, and others with the ability to save lives from opioid overdoses. Between 2013 and 2016, nine states instituted laws that give pharmacists direct authority to dispense naloxone to anyone without a prescription. However, the impact of such changes has remained rather unclear. Now, an NIH-funded analysis has found that within a couple of years of these new laws taking effect, fatal opioid overdoses in these states fell significantly [1].
The misuse and overuse of opioids, which include heroin, fentanyl, and prescription painkillers, poses an unprecedented public health crisis. Every day, more than 130 people in the United States die from opioid overdoses [2]. Not only are far too many families losing their loved ones, this crisis is costing our nation tens of billions of dollars a year in lost productivity and added expenses for healthcare, addiction treatment, and criminal justice.
Opioid overdoses lead to respiratory arrest. If not reversed in a few minutes, this will be fatal. In an effort to address this crisis, the federal government and many states have pursued various strategies to increase access to naloxone, which is a medication that can quickly restore breathing in a person overdosing on opioids. Naloxone, which can be delivered via nasal spray or injection, works by binding opioid receptors to reverse or block the effect of opioids. The challenge is to get naloxone to those who need it before it’s too late.
In some states, a physician still must prescribe naloxone. In others, naloxone access laws (NALs) have given pharmacists the authority to supply naloxone without a doctor’s orders. But not all NALs are the same.
Some NALs, including those in Alaska, California, Connecticut, Idaho, New Mexico, North Dakota, Oklahoma, Oregon, and South Carolina, give pharmacists direct authority to dispense naloxone to anyone who requests it. But NALs in certain other states only give pharmacists indirect authority to dispense naloxone to people enrolled in certain treatment programs, or who meet other specific criteria.
In the new analysis, published in JAMA Internal Medicine, a team that included Rahi Abouk, William Paterson University, Wayne, NJ, and Rosalie Liccardo Pacula and David Powell, RAND Corp., Arlington, VA, asked: Do state laws to improve naloxone access lead to reductions in fatal overdoses involving opioids? The answer appears to be “yes,” but success seems to hinge on the details of those laws.
The evidence shows that states allowing pharmacists direct authority to dispense naloxone to anyone have seen large increases in the dispensing of the medication. In contrast, states granting pharmacists’ only indirect authority to dispense naloxone have experienced little change.
Most importantly, the research team found that states that adopted direct authority NALs experienced far greater reductions in opioid-related deaths than states with indirect authority NALs or no NALs. Specifically, the analysis showed that in the year after direct authority NALs were enacted, fatal opioid overdoses in those states fell an average of 27 percent, with even steeper declines in ensuing years. Longer-term data are needed, and, as in all observational studies of this sort, one must be careful not to equate correlation with causation. But these findings are certainly encouraging.
There were some other intriguing trends. For instance, the researchers found that states that allow pharmacists to dispense naloxone without a prescription also saw an increase in the number of patients treated at emergency departments for nonfatal overdoses. This finding highlights the importance of combining strategies to improve naloxone access with other proven interventions and access to medications aimed to treat opioid addiction. Integration of all possible interventions is exactly the goal of the HEALing Communities Study mentioned above.
Successfully tackling the opioid epidemic will require a multi-pronged approach, including concerted efforts and research advances in overdose reversal, addiction treatment, and non-addictive pain management . As I’ve noted before, we cannot solve the opioid addiction and overdose crisis without finding innovative new ways to treat pain. The NIH is partnering with pharmaceutical industry leaders to accelerate this process, but it will take time. The good news based on this new study is that, with thoughtful strategies and policies in place, many of the tools needed to help address this epidemic and save lives may already be at our disposal.
References:
[1] Association Between State Laws Facilitating Pharmacy Distribution of Naloxone and Risk of Fatal Overdose. Abouk R, Pacula RL, Powell D. JAMA Intern Med. 2019 May 6
[2] Opioid Overdose Crisis. National Institute on Drug Abuse/NIH. Updated January 2019.
Links:
HEAL (Helping to End Addiction Long-Term) Initiative (NIH)
Naloxone for Opioid Overdose (National Institute on Drug Abuse/NIH)
NIH Support: National Institute on Drug Abuse
MicroED: From Powder to Structure in a Half-Hour
Posted on by Dr. Francis Collins
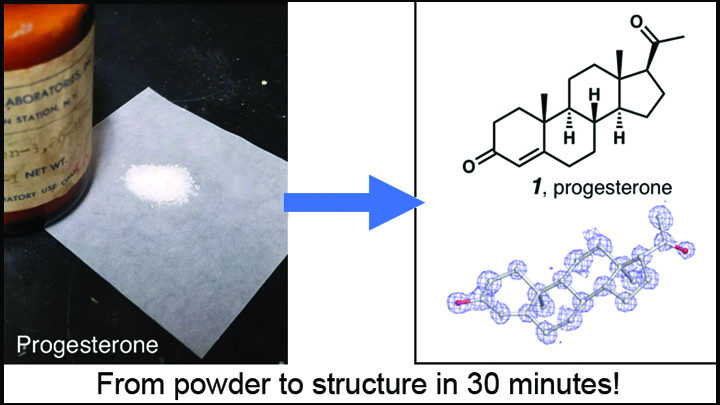
Credit: Adapted from Jones et al. ChemRxiv.org
Over the past few years, there’s been a great deal of excitement about the power of cryo-electron microscopy (cryo-EM) for mapping the structures of large biological molecules like proteins and nucleic acids. Now comes word of another absolutely incredible use of cryo-EM: determining with great ease and exquisite precision the structure of the smaller organic chemical compounds, or “small molecules,” that play such key roles in biological exploration and drug development.
The new advance involves a cryo-EM technique called microcrystal-electron diffraction (MicroED). As detailed in a preprint on ChemRxiv.org [1] and the journal Angewandte Chemie [2], MicroED has enabled researchers to take the powdered form of commercially available small molecules and generate high-resolution data on their chemical structures in less than a half-hour—dramatically faster than with traditional methods!
Creative Minds: Designing Personalized Clinical Trials
Posted on by Dr. Francis Collins

Karina Davidson/Credit: Jörg Meyer
It might have been 25 years ago, but Karina Davidson remembers that day like yesterday. She was an intern in clinical psychology, and two concerned parents walked into the hospital with their troubled, seven-year-old son. The boy was severely underweight at just 37 pounds and had been acting out violently toward himself and others. It seemed as though Ritalin, a drug commonly prescribed for Attention Deficit Disorder, might help. But would it?
To find out, the clinical team did something unconventional: they designed for the boy a clinical trial to test the benefit of Ritalin versus a placebo. The boy was randomly assigned to take either the drug or placebo each day for four weeks. As a controlled study, neither clinical staff nor the family knew whether he was taking the drug or placebo at any given time. The result: Ritalin wasn’t the answer. The boy was spared any side effects from long term administration of a medication that wouldn’t help him, and his doctors could turn to other potentially more beneficial approaches to his treatment.
Davidson, now an established clinical psychologist at the Columbia University Irving Medical Center, New York, wants to take the unconventional approach that helped this boy and make it more of the norm in medicine. With support from a 2017 NIH Director’s Transformative Research Award, she and her colleagues will develop three pilot computer applications—or digital platforms—to help doctors conduct one-person studies in their offices.
Creative Minds: Taking Aim at Adverse Drug Reactions
Posted on by Dr. Francis Collins

Sherrie Divito
As a practicing dermatologist, Sherrie Divito sees lots of patients each week at Brigham and Women’s Hospital, Boston. She also sees lots of research opportunities. One that grabbed her attention is graft-versus-host disease (GvHD), which can arise after a bone-marrow transplant for leukemia, lymphoma, or various other diseases. What happens is immune cells in the donated marrow recognize a transplant patient’s body as “foreign” and launch an attack. Skin is often attacked first, producing a severe rash that is a harbinger of complications to come in other parts of the body.
But Divito saw something else: it’s virtually impossible to distinguish between an acute GvHD-caused rash and a severe skin reaction to drugs, from amoxicillin to carbamazepine. In her GvHD studies, Divito had been researching a recently identified class of immune cell called tissue-resident memory T (Trm) cells. They remain in skin rather than circulating in the bloodstream. The clinical similarities made Divito wonder whether Trm cells may also help to drive severe skin allergies to drugs.
Divito has received a 2016 NIH Director’s Early Independence Award to find out. If correct, Divito will help not only to improve the lives of thousands of people with GvHD, but potentially benefit the millions of other folks who experience adverse reactions to drug.
Precision Medicine: Making Warfarin Safer
Posted on by Dr. Francis Collins
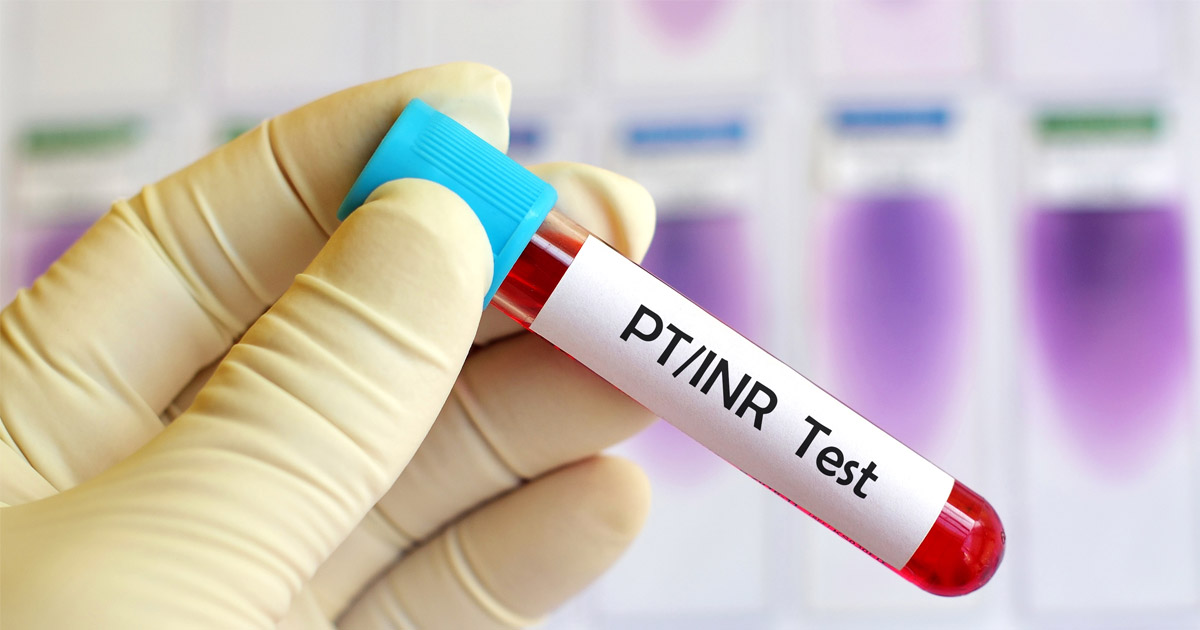
Caption: Finding the right dose of the drug warfarin can be tricky, even with this standard test to measure how fast a person’s blood clots.
Credit: Thinkstock/jarun011
Every year, thousands of older Americans require emergency treatment to stop bleeding caused by taking warfarin, a frequently prescribed blood-thinning pill. My own mother received this drug in her later years, and her doctors encountered significant challenges getting the dose right. The problem is too much warfarin causes potentially serious bleeding, while too little leaves those who need the drug vulnerable to developing life-threatening clots in their legs or heart. The difference between too little and too much is distressingly small. But what if before writing a prescription, doctors could test for known genetic markers to help them gauge the amount of warfarin that a person should take?
Such tests have been available to doctors and patients for a few years, but they have not been widely used. The recent results of a national clinical trial offer some of the most convincing evidence that it’s time for that to change. In this study of 1,650 older adults undergoing elective hip or knee surgery, patients whose genetic makeup was used to help determine their dose of warfarin were less likely to suffer adverse events, including major bleeding. This trial marks an encouraging success story for the emerging field of pharmacogenomics, the study of how the variations in our genes affect our responses to medicines.
Previous Page Next Page


