Chipping Away at the Causes of Polycystic Kidney Disease
Posted on by Lawrence Tabak, D.D.S., Ph.D.
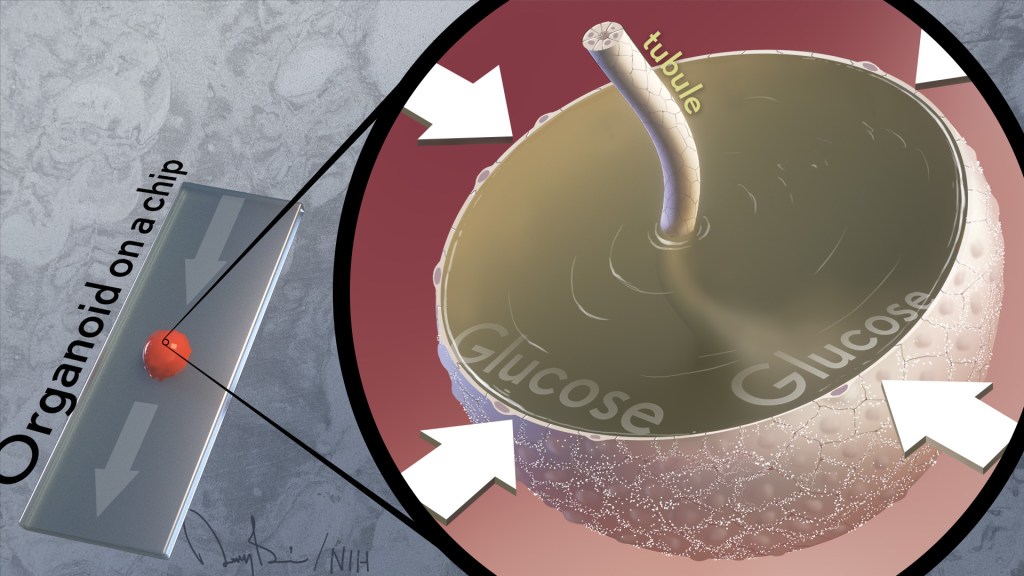
It’s often said that two is better than one. That’s true whether driving across the country, renovating a kitchen, or looking for a misplaced set of car keys. But a recent study shows this old saying also applies for modeling a kidney disease with two very complementary, cutting-edge technologies: an organoid, a living miniaturized organ grown in a laboratory dish; and an “organ-on-a-chip,” silicon chips specially engineered to mimic the 3D tissue structure and basic biology of a human body organ.
Using this one-two approach at the lab bench, the researchers modeled in just a few weeks different aspects of the fluid-filled cysts that form in polycystic kidney disease (PKD), a common cause of kidney failure. This is impossible to do in real-time in humans for a variety of technical reasons.
These powerful technologies revealed that blood glucose plays a role in causing the cysts. They also showed the cysts form via a different biological mechanism than previously thought. These new leads, if confirmed, offer a whole new way of thinking about PKD cysts, and more exciting, how to prevent or slow the disease in millions of people worldwide.
These latest findings, published in the journal Nature Communications, come from Benjamin Freedman and colleagues at the University of Washington School of Medicine, Seattle [1]. While much is known about the genetic causes of PKD, Freedman and team realized there’s much still much to learn about the basics of how cysts form in the kidney’s tiny tubes, or tubules, that help to filter toxins out of the bloodstream.
Each human kidney has millions of tubules, and in people with PKD, some of them expand gradually and abnormally to form sacs of fluid that researchers liken to water balloons. These sacs, or cysts, crowd out healthy tissue, leading over time to reduced kidney function and, in some instances, complete kidney failure.
To understand cyst formation better, Freedman’s team and others have invented methods to grow human kidney organoids, complete with a system of internal tubules. Impressively, organoids made from cells carrying mutations known to cause PKD develop cysts, just as people with these same mutations do. When suspended in fluid, the organoids also develop telltale signs of PKD even more dramatically, showing they are sensitive to changes in their environments.
At any given moment, about a quarter of all the fluids in the body pass through the kidneys, and this constant flow was missing from the organoid. That’s when Freedman and colleagues turned to their other modeling tool: a kidney-on-a-chip.
These more complex 3D models, containing living kidney cells, aim to mimic more fully the kidney and its environment. They also contain a network of microfluidic channels to replicate the natural flow of fluids in a living kidney. Combining PKD organoids with kidney-on-a-chip technology provided the best of both worlds.
Their studies found that exposing PKD organoid-on-a-chip models to a solution including water, glucose, amino acids, and other nutrients caused cysts to expand more quickly than they otherwise would. However, the cysts don’t develop from fluids that the kidneys outwardly secrete, as long thought. The new findings reveal just the opposite. The PKD cysts arise and grow as the kidney tissue works to retain most of the fluids that constantly pass through them.
They also found out why: the cysts were absorbing glucose and taking in water from the fluid passing over them, causing the cysts to expand. Although scientists had known that kidneys absorb glucose, they’d never connected this process to the formation of cysts in PKD.
In further studies, the scientists gave fluorescently labeled glucose to mice with PKD and could see that kidney cysts in the animals also took up glucose. The researchers think that the tubules are taking in fluid in the mice just as they do in the organoids.
Understanding the mechanisms of PKD can point to new ways to treat it. Indeed, the research team showed adding compounds that block the transport of glucose also prevented cyst growth. Freedman notes that glucose transport inhibitors (flozins), a class of oral drugs now used to treat diabetes, are in development for other types of kidney disease. He said the new findings suggest glucose transport inhibitors might have benefits for treating PKD, too.
There’s much more work to do. But the hope is that these new insights into PKD biology will lead to promising ways to prevent or treat this genetic condition that now threatens the lives of far too many loved ones in so many families.
This two-is-better-than-one approach is just an example of the ways in which NIH-supported efforts in tissue chips are evolving to better model human disease. That includes NIH’s National Center for Advancing Translational Science’s Tissue Chip for Drug Screening program, which is enabling promising new approaches to study human diseases affecting organ systems throughout the body.
Reference:
[1] Glucose absorption drives cystogenesis in a human organoid-on-chip model of polycystic kidney disease. Li SR, Gulieva RE, Helms L, Cruz NM, Vincent T, Fu H, Himmelfarb J, Freedman BS. Nat Commun. 2022 Dec 23;13(1):7918.
Links:
Polycystic Kidney Disease (National Institute of Diabetes and Digestive and Kidney Diseases/NIH)
Your Kidneys & How They Work (NIDDK)
Freedman Lab (University of Washington, Seattle)
Tissue Chip for Drug Screening (National Center for Advancing Translational Sciences/NIH)
NIH Support: National Center for Advancing Translational Sciences; National Institute of Diabetes and Digestive and Kidney Diseases; National Heart, Lung, and Blood Institute

My grandfather said radishes are good for your kidneys, so I eat one Monday thru Friday!
High blood pressure and diabetes are the two most common causes of kidney failure. With proper treatment kidney diseases are cured.
This important study on the pathogenesis of polycystic kidney leads us to ask whether this method can be applied for Polycystic Liver. Part of this result achieved on renal tissue microstructures will have something in common in development also in the pathogenesis of liver cysts (inherited genetic disorders).