COVID-19 Infected Many More Americans in 2020 than Official Tallies Show
Posted on by Dr. Francis Collins
At the end of last year, you may recall hearing news reports that the number of COVID-19 cases in the United States had topped 20 million. While that number came as truly sobering news, it also likely was an underestimate. Many cases went undetected due to limited testing early in the year and a large number of infections that produced mild or no symptoms.
Now, a recent article published in Nature offers a more-comprehensive estimate that puts the true number of infections by the end of 2020 at more than 100 million [1]. That’s equal to just under a third of the U.S. population of 328 million. This revised number shows just how rapidly this novel coronavirus spread through the country last year. It also brings home just how timely the vaccines have been—and continue to be in 2021—to protect our nation’s health in this time of pandemic.
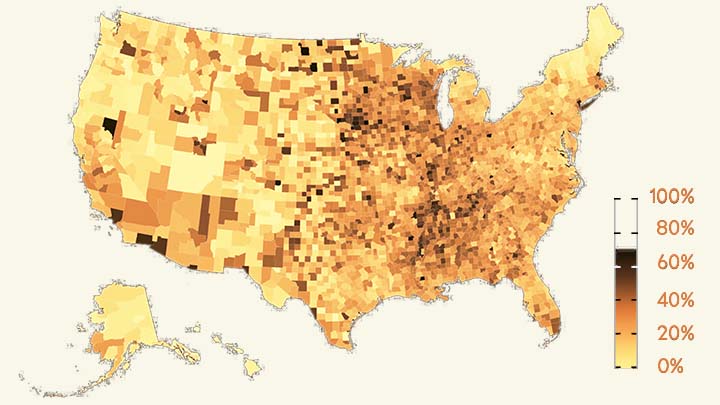
The work comes from NIH grantee Jeffrey Shaman, Sen Pei, and colleagues, Columbia University, New York. As shown above in the map, the researchers estimated the percentage of people who had been infected with SARS-CoV-2, the novel coronavirus that causes COVID-19, in communities across the country through December 2020.
To generate this map, they started with existing national data on the number of coronavirus cases (both detected and undetected) in 3,142 U.S. counties and major metropolitan areas. They then factored in data from the Centers for Disease Control and Prevention (CDC) on the number of people who tested positive for antibodies against SARS-CoV-2. These CDC data are useful for picking up on past infections, including those that went undetected.
From these data, the researchers calculated that only about 11 percent of all COVID-19 cases were confirmed by a positive test result in March 2020. By the end of the year, with testing improvements and heightened public awareness of COVID-19, the ascertainment rate (the number of infections that were known versus unknown) rose to about 25 percent on average. This measure also varied a lot across the country. For instance, the ascertainment rates in Miami and Phoenix were higher than the national average, while rates in New York City, Los Angeles, and Chicago were lower than average.
How many people were potentially walking around with a contagious SARS-CoV-2 infection? The model helps to answer this, too. On December 31, 2020, the researchers estimate that 0.77 percent of the U.S. population had a contagious infection. That’s about 1 in every 130 people on average. In some places, it was much higher. In Los Angeles, for example, nearly 1 in 40 (or 2.42 percent) had a SARS-CoV-2 infection as they rang in the New Year.
Over the course of the year, the fatality rate associated with COVID-19 dropped, at least in part due to earlier diagnosis and advances in treatment. The fatality rate went from 0.77 percent in April to 0.31 percent in December. While this is great news, it still shows that COVID-19 remains much more dangerous than seasonal influenza (which has a fatality rate of 0.08 percent).
Today, the landscape has changed considerably. Vaccines are now widely available, giving many more people immune protection without ever having to get infected. And yet, the rise of the Delta and other variants means that breakthrough infections and reinfections—which the researchers didn’t account for in their model—have become a much bigger concern.
Looking ahead to the end of 2021, Americans must continue to do everything they can to protect their communities from the spread of this terrible virus. That means getting vaccinated if you haven’t already, staying home and getting tested if you’ve got symptoms or know of an exposure, and taking other measures to keep yourself and your loved ones safe and well. These measures we take now will influence the infection rates and susceptibility to SARS-CoV-2 in our communities going forward. That will determine what the map of SARS-CoV-2 infections will look like in 2021 and beyond and, ultimately, how soon we can finally put this pandemic behind us.
Reference:
[1] Burden and characteristics of COVID-19 in the United States during 2020. Pei S, Yamana TK, Kandula S, Galanti M, Shaman J. Nature. 2021 Aug 26.
Links:
COVID-19 Research (NIH)
Sen Pei (Columbia University, New York)
Jeffrey Shaman (Columbia University, New York)

If we had about 100M people who’d been infected by the end of 2020 – and very high numbers in January 2021- going lower for about six months until June – but now soaring again with the Delta variant – shouldn’t we have about 200M previously infected by now? Let’s say 165M – 1/2 US population -and we have about 50% vaccination rate of eligible people that means about 75% of people eligible for a vaccine should have some immunity – they were either vaccinated or infected.
With 75%, I would think we would have, if not herd immunity, at least a big resistance to another epidemic – but looking at the mortality rate lately, it is not low, it’s about 1/2 of the most lethal days, which were the 2nd week of January 2021. Peak deaths per day were a bit over 3,000 back then, and now we have 1,500.
I do understand many people are unvaccinated, and I understand some people are burned out on masks and distancing, and this Delta variant is more contagious, but still I wonder.
So if there were 100 million cases by 2020 and we have vaccinated around 165 million why are we not approaching herd immunity???
Well, for starters, those two groups are not completely separate, but instead likely largely overlap on the Venn Diagram. I belong to both for instance.
I will say that — trusting estimates that perhaps roughly 50% of the population now has some degree of natural immunity — we should probably expect that pretty soon we will begin to see longer-term resistance to disproportionately bad outcomes from this disease. At least, I should hope this is true. Vaccination may be a short- to medium-term solution when this is all said and done, but natural immunity will hopefully persist and help prevent more severe outcomes (and, according to some recent research, maybe a significant percentage of symptomatic cases) in the longer run also.
My hope is that Delta is the final really nasty wave we see of this pathogen. Probably I’m wrong, and probably it’s wishful thinking, but given the growth in overall infection/recovery rates + vaccination it all has to add up to more community resistance to the disease going forward.
I’ve seen estimates of R0 for the Delta variant ranging as low as 5 and as high as 9. Therefore, herd immunity would require 80% – 89% of the population to be immune, either from natural immunity or from vaccination. That would mean 265-295 million with protective immunity would be required to reach herd immunity in the US.
About 15% of the US population is younger than 12 and currently not eligible for vaccination. Some of them have been infected, of course, but the evidence shows that natural immunity is likely to develop and be durable if the severity of the infection is at least moderate to severe (though very severe sometimes results in poor natural immunity). Children typically have mild symptoms (if any), with notable exceptions (of course), so I would not count on a high proportion of those under 12 to have protective immunity, even with a history of past infection. Additionally, even adults can fail to develop, or can lose, protective natural immunity after infections, 7-16% in the SIREN study.
For those vaccinated, the immunity is waning to some extent. Though vaccines continue to substantially protect against hospitalization and death, breakthrough infections are increasing relative to the earlier variants. Those with breakthrough infections can certainly transmit the infection to others, though fortunately they appear to have a shorter duration of transmissibility than those unvaccinated and infected.
So, I think of it kind of like 3 steps forward and 1 step backward as far as natural and vaccine-induced immunity are concerned. Assuming a variant does not arise that significantly evades the 2 types of immunity, we’ll get there eventually. Unfortunately, until the whole world acquires protective immunity, the possibility of evasive variants looms large.
Would be an interesting experiment to perform antibody tests among the ineligible age groups and then more accurate projections could be made as to how complete the vaccination effort has to be among the eligible but remaining unvaccinated non-infected American adults.
As far as I know, a positive SARS-CoV-2 antibody in itself would not necessarily demonstrate protective immunity against reinfection for those currently ineligible for vaccinations. There likely is a minimum titer of antibody that would be needed to be protective, but I am not aware of what that titer is or would be. It’s entirely possible, of course, that the information is known and I’m simply unaware of it.
And herd immunity may not rely entirely only on humoral immunity; cell-mediated immunity likely has a role to play, but that is more difficult to study and, again, to my knowledge, has not been ascertained in terms of specific parameters.
Everything I’ve ever read during my years reading the medical literature says that you must have at least 90% of the population immune to have herd immunity. And since people who have had COVID have gotten it again (another variant) that doesn’t necessarily give you immunity.
Because infection doesn’t assure immunity to reinfection (not even close, and neither do the vaccines)
Personally the way this virus has been able to change into other variants is of great concern. I would also like to add that my observation out in the community seems to be of less concern. For example, most people are not using masks, or even being as sanitary as from the start.
I agree. I think masks work more than people give them credit for.
Is there a link to an interactive map where I can zoom in, see state lines, see data by county…?
I Like It. Good one
Studies continue to prove natural immunity is stronger, more wide ranging and lasts longer than the vaccines. Why are those with natural immunity being forced to get the vaccines? We also have more therapeutics to help overcome this disease. Why is our government pushing this on healthy people? Makes No sense! Control?
I received 2 doses of Moderna VAX(1st to 2nd dose took me 3 months due to unforeseen circumstances. I am considered vaxed. What is your opinion on virus protection with 3 months instead of 1 month in between? ALSO SIDE EFFECTS WERE MUCH LESS THAN 1ST SHOT, WHEREAS THEY SAID THE 2ND IS USUALLY WORSE THAN THE 1ST IN TERMS OF SIDE EFFECTS.
My daughter was 16 at the time of her infection back in October. Lost both Smell and Taste. Taste returned – altered. Smell pops back in for an hour or two over a weeks time, but is basically gone. She tested positive for Covid. She has had 20+ retests and has never tested positive in basically a year. (Job requires LOTS of testing.) Why should she have to get vaccinated? Immunity is immunity right? Again, she is still dealing with the aftermath. So something is obviously still going on. I just do not understand how a lab created immunity can be better than what is now a natural immunity. (Tcell test.)
I am not aware of any commercially available T cell test that provides any definitive information about one’s protective cell-mediated immunity. The one of which I am aware states on its website that, for a positive test, “the implications for immunity are not known.” Its only value currently claimed is to verify that one has had a SARS-CoV-2 infection.
Additionally, there are reports of those (about a third) with ongoing symptoms secondary to a previous COVID-19 infection substantially improving after vaccination. Admittedly, there is a much smaller percentage (about 4%) who seemed to worsen after vaccination.
Have any of you noticed the dramatic decrease in flu cases lately? Do the math folks.
I wish the general pubic could understand and leadership admit that there is no such thing as beating the virus (for example the flu has never been beaten) and quit using that term. Its misleading, inaccurate and as long as we have humans and animal host on this planet its here to stay.
This is from an engineer’s point of view so my take on it is a bit different. I think we’re on the same path however — our goals is to get this under control.
First problem is the majority of masks do nothing. Coupled with the fact people are wearing them improperly and wearing them over facial hair, masks are a huge waste of time. Thin poorly fitted pieces of fabric and pieces of thin paper do little to nothing to stop the spread.
Second problem: Social media. I visit worksites set up not according to CDC guidelines but according to guidance from Reddit, Facebook and Twitter. Believe it or not, we have a fairly good grasp on how this spreads and what is needed to contain it. And if we don’t do those things, instead we … set up work areas that do not isolate/contain people and circulate clean air, we’re just spreading the illness.
Less focus needs to be put on wiping surfaces with bleach every 30 min and more on ensuring air circulation brings fresh uncontaminated air to workers.
It’s a respiratory illness with a very short lifespan when it lands on a surface. That’s not the problem. Problem the airborne phase and controlling that.
And we’re not doing a good job of it AT ALL. People need to spend less time getting advice from social media platforms and actually understanding what we are dealing with.
40 years of wearing masks, self-contained breathers, filters and other PPE tells me that if we can get people to stop wasting time on paper and cloth and wear actual filter masks (properly fitted) we could bring numbers down rapidly.
But what do I know, right? I’m not social media …
The “paper” surgical masks are actually made of a plastic polymer. I’ve read it can develop enough electrostatic charge to attract and hold virus particles. In fact, a study done in Bangladesh indicates the surgical masks are far superior to cloth ones for reducing spread of the virus. Of course, N95s are the best, and even if not fit tested tend to provide very good protection.
We are still using our masks when in public and I wash down the grocery cart before using it. We had our original 2nd vaccines April 1 & 2. 2021. I had the virus in Feb. 2020. Worse sickness I ever had.
If 100 million have been infected, and, according to CDC, 175 million have been vaccinated, than a total of 275 million Americans should be immunized at present. This would be 83% of 328 million Americans living today in the US. In conclusion: if the required herd immunity has been estimated at at least 85% immunized population, the US should be seeing soon a significant drop in hospital admissions.
that is exactly what I said 2 days ago
The vaccinated group and the infected group overlap.
Those numbers are not mutually exclusive …
And immunity is not permanent, nor 100% in either those with an infection or in those vaccinated.
To completely solve the problem of COVID 19, we need to understand the key problem at the cell membrane: when the cell membrane is opened, the intracellular and extracellular fluid are regulated, biochemical reactions are regulated uniform, the voltage inside and outside the cell is stabilized… this makes the virus activity optimal, unobstructed, does not cause blockage at the cell membrane leading to cell destruction; does not cause the phenomenon of “short circuit” because receptors and viruses spike causing blockage in the cell membrane . . .
What we all need now in order to feel better are easy answers. Surely there must be a long line of politicians with ample supplies…
If the true infection rate is 100M Americans and the death rate is the stated 680K (as at 2021-09-14 AM) then the true CFR is .0068. Sounds a lot like the flu to me. Is our risk aversion a problem
That is not what a case fatality ratio measures. The infection fatality ratio (IFR) estimates the proportion of deaths among all infected individuals. The case fatality ratio (CFR) estimates the proportion of deaths among identified confirmed cases. What you’re referring to is more properly the IFR.
This is not the flu. Estimates of the reproduction number (R0) of the influenza virus during pandemics yields the highest estimate of 1.47–2.27 for the 1918 pandemic. The R0 for the Delta variant has yielded estimates of 5–9. It is much more contagious than any influenza we’ve likely seen and, as a result, is infecting many more people and, as a further consequence, is killing many more people.
Sometimes (as, I contend, in the case of SARS-CoV-2), risk aversion is rational and prudent.
Thanks for your answer. However, I am still bemused. I am a retired CPA so I look at ratios and think very simply that if >100M people get a disease and there are ~680K confirmed deaths, that means that the present probability of death from the disease is 0.68% or inverted, you have a 99.32% probability of survival. Is that not correct? If I am missing something important I would like to know. I know that this is an over simplification and that the probabilities stratify with age cohorts and comorbidities, etc.
You’re welcome.
All in all, I don’t think you’re far off. The only addition I’d make is that the number of deaths (the numerator) used in the 2 ratios is the number of confirmed deaths. The denominator is the total number of cases, estimated (IFR) or confirmed (CFR). The number of deaths may be greater than the number of confirmed deaths, so both ratios may be greater than the official numbers. Even if my presumption is correct, I doubt it would alter the ratios all that much.
I can’t speak for you, of course, but many seem to be focusing on the survival rate of 97-99% (+/-) and, therefore, thinking/writing/saying “What’s the big deal?” In my opinion, focusing on the survival rate misses several important points.
(1) Because this virus is as contagious as it is (R0 of 5-9), it has infected, is infecting, and will infect a wide swath of the population, so the absolute numbers (not the percentage) of infected people and resultant deaths is and will be very large. For a perspective that may be helpful, consider that, just in the USA alone, the number of citizens killed by this pandemic exceeds (by more than 162,000, and rising) the total number of US citizens killed on 9/11 (2,977), in the Korean War (33,686), in the Vietnam War (58,220), and in World War II (405,399).
(2) Focusing only on the survival rate ignores the known, life-altering (for many) disability known as “long COVID” which afflicts somewhere between 10–30% of those infected.
(3) There may be unknown consequences of the residual effects of having had this viral infection years or decades from now. There may be none, there may be many. Thinking that those who survive the infection will be good to go is not necessarily true.
Thanks for your comments. It occurs to me that there are also unknown consequences of the vaccine. Bad signs are arising. Teenage boys are a cohort that appears to be reacting badly to the vaccine. Myocarditis and Pericarditis seem to be a problem for them. Given the extremely low CFR in this cohort it appears that “the cure is worse than the disease”. This makes me think that the doctors who wrote the Great Barrington declaration were really on to something.
Yes, possible unknown consequences of the vaccines, but if history is any guide, most adverse consequences of vaccines are seen within the first couple of months after administration, whereas the adverse consequences of viral infections can occur months, years, or decades after the infection (think herpes simplex, varicella/zoster, HPV, Epstein-Barr).
Regarding the myocardial and pericardial effects of the vaccines, there was a very good article about that subject published yesterday (9/13/2021) by an epidemiologist, Katelyn Jetelina, MPH, PhD.
If interested, search for “Your Local Epidemiologist Myocarditis, preprints, and the UK”
Also with regard to the safety of the vaccines, a study from Israel of the Pfizer vaccine (published in the New England Journal of Medicine August 25, 2021; see “Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting”) showed some safety concerns (including, as you mentioned, myocarditis), but compared to the adverse effects of a SARS-CoV-2 infection, the vaccination risks (including myocarditis) were far less.
You are missing something very important here. The death rates go way up with age. If it killed 30% of 1 year olds and no one else it would also have a 0% chance of killing you. But, we would be using the national guard to vaccinate everyone and incarcerating anyone without a mask.
Which means we have a lot more naturally immune people around than we thought. Let’s recognize the multiple studies supporting on par if not better immunity post infection versus post inoculation.
There likely are more naturally immune people than we recognize, but understand that neither having an infection nor having a complete series of vaccinations necessarily results in protective immunity. Regarding natural immunity, studies have shown that (in general) the robustness of one’s protective natural immunity is dependent on the severity of the infection (though very severe infections sometimes result in subpar immunity). Those with asymptomatic infections may have had a minimal immune response, that response may fade over time, and it might be relatively specific for the variant that caused the original infection.
Have you seen the just completed Israeli study that shows that naturally acquired immunity is up to 13X more protective than vaccine acquired protection and it also has a significantly longer decay curve?
No, I haven’t seen that. Can you provide details so I may find it? This site does not support URLs, so the actual name of the study and the name of the website would be best.
I’m curious how they selected those with natural immunity, whether they did so via serology (which would likely include those with asymptomatic infections) or those only with symptomatic illness subsequently confirmed with an antigen or PCR test (which likely would include few, if any, with asymptomatic infections). That would make a big difference in the ability to generalize the importance of those findings to the population of those infected.
This is the title of the article. Use it. It pops up first. Having SARS-CoV-2 once confers much greater immunity than a vaccine—but vaccination remains vital
Thanks for the information on that Israeli study. From the article:
The study, conducted in one of the most highly COVID-19–vaccinated countries in the world, examined medical records of tens of thousands of Israelis, charting their infections, symptoms, and hospitalizations between 1 June and 14 August, when the Delta variant predominated in Israel.
“The biggest limitation in the study is that testing [for SARS-CoV-2 infection] is still a voluntary thing—it’s not part of the study design.” That means, she says, that comparisons could be confounded if, for example, previously infected people who developed mild symptoms were less likely to get tested than vaccinated people, perhaps because they think they are immune.
This strongly suggests that the studied population of those with natural immunity was not a random selection of all those who had experienced a SARS-CoV-2 infection, but was of those with a medical record that would have recorded their positive test based on symptoms and/or hospitalizations. If so, then it would omit the likely large(r) number of those with asymptomatic and unconfirmed infections whose natural immunity may be meager, nonexistent or transient.
It is, of course, good to see that those unfortunate enough to experience a symptomatic SARS-CoV-2 infection have a relatively high degree of protection against reinfection (especially if they receive at least one dose of a vaccine), but the study does not generalize to all of those with SARS-CoV-2 infections, since those with asymptomatic infections may not be afforded such high levels of immunity.
Get Vaccinated & follow all the rules strictly then we will overcome this pandemic situation…
Is it possible that the immunity conferred by the mRNA vaccine, being, ingeniously, targeted to the spike proteins of the predominant form of the virus does not confer as robust immunity to delta and other forms due to mutations in the spike proteins? The plus here is that if the original form had been encountered after vaccination, the spike proteins would be stripped away/disabled, and the rest of the virus would be destroyed by the immune system, thereby conferring an immunity to the capsule proteins and internal contents which are likely to be similar in succeeding variants.
That is, of course, an important question you pose. I don’t think anyone knows for sure at this point, though there is evidence that the vaccines target more sites on the receptor-binding domain (RBD) than the immunity generated by natural infection (see “How Immunity Generated from COVID-19 Vaccines Differs from an Infection” in this NIH Director’s Blog from June 22, 2021, as well as an earlier article from June 4, 2021 (Science, titled “Prevalent, protective, and convergent IgG recognition of SARS-CoV-2 non-RBD spike epitopes”) which found in a small study that the neutralizing antibodies in those who had had a SARS-CoV-2 infection were primarily directed against the N-terminal domain (NTD) of the virus. The NTD mutates very frequently; changes in the NTD are responsible for many of the variants of concern, so immunity induced by the vaccines may function better against the variants than the immunity induced by natural infection.
Great Post!! Thanks for sharing this informative blog.