How Severe COVID-19 Can Tragically Lead to Lung Failure and Death
Posted on by Dr. Francis Collins
More than 3 million people around the world, now tragically including thousands every day in India, have lost their lives to severe COVID-19. Though incredible progress has been made in a little more than a year to develop effective vaccines, diagnostic tests, and treatments, there’s still much we don’t know about what precisely happens in the lungs and other parts of the body that leads to lethal outcomes.
Two recent studies in the journal Nature provide some of the most-detailed analyses yet about the effects on the human body of SARS-CoV-2, the coronavirus that causes COVID-19 [1,2]. The research shows that in people with advanced infections, SARS-CoV-2 often unleashes a devastating series of host events in the lungs prior to death. These events include runaway inflammation and rampant tissue destruction that the lungs cannot repair.
Both studies were supported by NIH. One comes from a team led by Benjamin Izar, Columbia University, New York. The other involves a group led by Aviv Regev, now at Genentech, and formerly at Broad Institute of MIT and Harvard, Cambridge, MA.
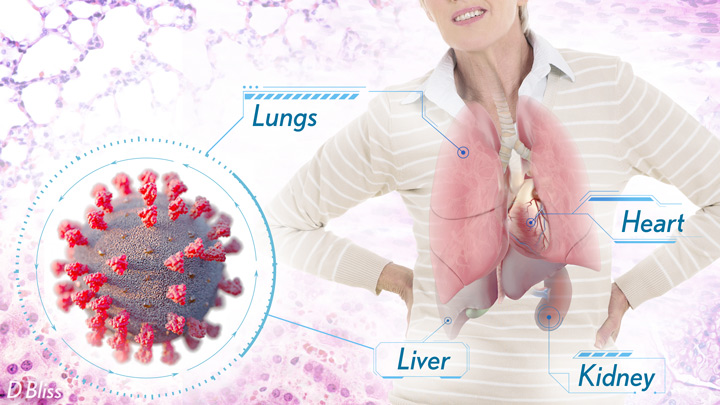
Each team analyzed samples of essential tissues gathered from COVID-19 patients shortly after their deaths. Izar’s team set up a rapid autopsy program to collect and freeze samples within hours of death. He and his team performed single-cell RNA sequencing on about 116,000 cells from the lung tissue of 19 men and women. Similarly, Regev’s team developed an autopsy biobank that included 420 total samples from 11 organ systems, which were used to generate multiple single-cell atlases of tissues from the lung, kidney, liver, and heart.
Izar’s team found that the lungs of people who died of COVID-19 were filled with immune cells called macrophages. While macrophages normally help to fight an infectious virus, they seemed in this case to produce a vicious cycle of severe inflammation that further damaged lung tissue. The researchers also discovered that the macrophages produced high levels of IL-1β, a type of small inflammatory protein called a cytokine. This suggests that drugs to reduce effects of IL-1β might have promise to control lung inflammation in the sickest patients.
As a person clears and recovers from a typical respiratory infection, such as the flu, the lung repairs the damage. But in severe COVID-19, both studies suggest this isn’t always possible. Not only does SARS-CoV-2 destroy cells within air sacs, called alveoli, that are essential for the exchange of oxygen and carbon dioxide, but the unchecked inflammation apparently also impairs remaining cells from repairing the damage. In fact, the lungs’ regenerative cells are suspended in a kind of reparative limbo, unable to complete the last steps needed to replace healthy alveolar tissue.
In both studies, the lung tissue also contained an unusually large number of fibroblast cells. Izar’s team went a step further to show increased numbers of a specific type of pathological fibroblast, which likely drives the rapid lung scarring (pulmonary fibrosis) seen in severe COVID-19. The findings point to specific fibroblast proteins that may serve as drug targets to block deleterious effects.
Regev’s team also describes how the virus affects other parts of the body. One surprising discovery was there was scant evidence of direct SARS-CoV-2 infection in the liver, kidney, or heart tissue of the deceased. Yet, a closer look heart tissue revealed widespread damage, documenting that many different coronary cell types had altered their genetic programs. It’s still to be determined if that’s because the virus had already been cleared from the heart prior to death. Alternatively, the heart damage might not be caused directly by SARS-CoV-2, and may arise from secondary immune and/or metabolic disruptions.
Together, these two studies provide clearer pictures of the pathology in the most severe and lethal cases of COVID-19. The data from these cell atlases has been made freely available for other researchers around the world to explore and analyze. The hope is that these vast data sets, together with future analyses and studies of people who’ve tragically lost their lives to this pandemic, will improve our understanding of long-term complications in patients who’ve survived. They also will now serve as an important foundational resource for the development of promising therapies, with the goal of preventing future complications and deaths due to COVID-19.
References:
[1] A molecular single-cell lung atlas of lethal COVID-19. Melms JC, Biermann J, Huang H, Wang Y, Nair A, Tagore S, Katsyv I, Rendeiro AF, Amin AD, Schapiro D, Frangieh CJ, Luoma AM, Filliol A, Fang Y, Ravichandran H, Clausi MG, Alba GA, Rogava M, Chen SW, Ho P, Montoro DT, Kornberg AE, Han AS, Bakhoum MF, Anandasabapathy N, Suárez-Fariñas M, Bakhoum SF, Bram Y, Borczuk A, Guo XV, Lefkowitch JH, Marboe C, Lagana SM, Del Portillo A, Zorn E, Markowitz GS, Schwabe RF, Schwartz RE, Elemento O, Saqi A, Hibshoosh H, Que J, Izar B. Nature. 2021 Apr 29.
[2] COVID-19 tissue atlases reveal SARS-CoV-2 pathology and cellular targets. Delorey TM, Ziegler CGK, Heimberg G, Normand R, Shalek AK, Villani AC, Rozenblatt-Rosen O, Regev A. et al. Nature. 2021 Apr 29.
Links:
COVID-19 Research (NIH)
Izar Lab (Columbia University, New York)
Aviv Regev (Genentech, South San Francisco, CA)
NIH Support: National Center for Advancing Translational Sciences; National Heart, Lung, and Blood Institute; National Cancer Institute; National Institute of Allergy and Infectious Diseases; National Institute of Diabetes and Digestive and Kidney Diseases; National Human Genome Research Institute; National Institute of Mental Health; National Institute on Alcohol Abuse and Alcoholism

I am confused. In Dr. Collins 8th paragraph he says “one surprising discovery” of Regev’s team was finding “scant” evidence of infection in the liver, kidney, or heart tissue.” Then on “closer” look, there was . . . and he proceeds to describe problems with the heart. Going from “scant” to significant, all in one paragraph. is a difficult logical jump for me, as a lay person. It makes me feel like I’m missing a huge gap.
Thanks for your comment, Barbara. The original sentence refers to signs of active infection in those organs at the time of death. But in the heart, the researchers detected signs of tissue damage but no active infection. As the paragraph’s final two sentences note, “It’s still to be determined if that’s because the virus had already been cleared from the heart prior to death. Alternatively, the heart damage might not be caused directly by SARS-CoV-2, and may arise from secondary immune and/or metabolic disruptions.” I hope this helps, and thanks again for asking.
Thank you Moderator for your quick reply. One follow up question? I think I misinterpreted what is “active infection at the time of death”. So “active infection” means the virus is visible, where in the heart there was no visible virus but there were signs of it having possibly been there?
Barbara, that’s right. There were signs that the virus possibly infected heart tissue at some point. But it’s still to be determined.
Thank you from this reader as well. That was my question too and I appreciate your answer.
Why haven’t we heard more about ExoFlo (extracellular vesicles containing messinger RNA)? I believe it is finishing Phase Ii trial and is available via emergency use; is said to be anti-inflammatory and fight cytokines
Very interesting, will follow up
Thank You
If IL-1b is causing lung pathology, how about treating Covid-19 patients with IL-1b antagonist, sIL-1Ra (aka Anakinra aka Kinaret) which is routinely used to treat Rheumatoid Arthritis patients? This will also avoid administering high doses immunosuppressive steroids to Covid-19 patients.
All you need is Aviptadil or Zyesami. Should be available soon and part of our standard of care. It’s not a vaccine but a therapeutic. Are you familiar with it?
Aviptadil is available under Compassionate use, so if you know someone on a vent ask for Aviptadil. It works!
Zyesami, also called Aviptadil, or RLF-100, a sythetic version of the naturally occurring human and mammalian Vasoactive Intestinal Peptide, is the only therapeutic that has been shown to be significantly effective in the critical stages of ARDS. With over 3 million dead so far, and the Covid-19 still killing so many, it is a wonder why this has not garnered further attention. For the next possible 3 million or so, it is life or death.
Previous research has shown that high dose intravenous vitamin C (HDIVC) benefits patients with sepsis, acute lung injury (ALI), the acute respiratory distress syndrome (ARDS), and early administration of HDIVC could prevent progression to ARDS, but it looks to me that vitamin C and HDIVC are shunned.
HDIVC could have saved the lives of tens of thousands of COVID-19 infected people.
There have been enough clinical trials which support this.
Vitamin C supports the leukocytes which are essential to fight infections, and high dose intravenous vitamin C injections are able to avoid intubation, to avoid sepsis and to reduce ICU time.
My son steven, who was a nurse practitioner and had been on life flight for many years. He was also president of ASTNA. Steve was exposed to Covid before Thanksgiving 2020. He tried self medicating himself until he felt the need to go to the hospital. His ex rays and blood work was not good. He was put in ICU on 100% oxygen. They tried infusion and experimental drugs. They went to proning. He was not showing any improvement. He had no prior health issues. They intubated him and then went to the Ecmo machine. We were told all his vitals and organs were good. Dec 29, 2020 we got the call his heart gave out and he passed away.. Here is my question how can the heart give out when the rest of the organs look good. Steve did have ARDS and he told me if they can’t clear it up you die. He did deal with low blood pressure through this. He said it was like your drowning in a pool and you can’t get any air. I’m in shock he went so fast. I really believed he was going to make it. Why do smokers get it and they are fine in a couple of weeks since they have done damage to their lungs, versus those who don’t?
I may be late answering this, and keep in mind I’m not a doctor or anything, but the heart and lungs are closely related.
When their are problems with the lungs and it becomes difficult to breathe, your heart has to work harder to keep blood flowing through your body. From what I understand, the infection from Covid is likely filling the lungs with fluid and thus making breathing harder.
Mucus is a defence mechanism. You’re body produces it to move particulates out of the lungs. However, mucus congests your lungs and makes it harder for you to take easy breaths of oxygen. Mucus is fine, it’s not likely to stress your heart out too much, but the reaction that bodies are having to fighting Covid may be immense by comparison.
Your heart is a muscle. It’s used to beating at a certain pace. If your son was on 100% oxygen to try to get oxygen in the lungs, and then put on a respirator, it’s likely that his heart was working overtime that whole time. It’s possible that even though the other organs were not damaged by the virus, that the heart simply could not put up with the added demand of trying to pump oxygen through the blood.
It’s come to me that counting those who have gotten COVID-19 and recovered, presumably with antibodies against it, with those who have been vaccinated should be bringing us a lot closer to herd immunity than we think we are. Could this be true or am I missing something?
Could you explain reasons why one should get the vaccine if they have had COVID-19?
Dr. Fauci was asked that today on CSPAN. I am no expert and I’m not the moderator, but I did want to share that in his answer he said that getting the vaccine, after having had covid, gives you protection against variants. He might also have said that they don’t know how long the protection from an active case of covid lasts, but that the vaccine prompts good antibody and T cell immunity.
Was wondering if these people that died so tragically from getting covid- were they testing negatively like the testing said they didn’t have covid anymore? All the while reaping havoc in the organ? Were some of these people thinking they were free and clear of covid before damage severity caused death??
April that is my question as well. I had Covid and the first thing it attacked was my lungs due to my chronic asthma. I also developed pneumonia. now I’m still struggling with breathing and trying to see if my lungs are even more damaged since Covid.. while having COVID my blood pressure was lower, and I did not have to take any medication. I’ve suffered with hypertension for over 18 years….
Thank you for sharing the information above. Mainly thank you for the attempt to spread explanations based on recent work on COVID issue.
I have a suggestion similar to the one made above for IL-1b. Why don’t we use the medications “pirfenidone (Esbriet) OR nintedanib (Ofev)” recommended for “pulmonary fibrosis”, at the early stages of Oxygen level drop detection. As there is not much cough detected in COVID patients, it is likely that these medications could prevent the breathing problem, considering the person has normal health condition . . .
Thank you very much for the information.
Vaccination is one component of pandemic management. At home tests . . . address another behavioral aspect of how to minimize spread, especially as vaccination may result in asymptomatic spread of potential variants. Next time you use that smart phone, realize that it knows a lot more of your behavior than you suspect.
Why we should continue to be vigilant as covid rages in other parts of the world. Especially when vaccination rates continue to be low among marines and other military personnel.
Amazing and scientifically stimulating SARS-Covid-19 update with convincing research data-set amalgamating death-trends and disproportionate share of morbidity and mortality amongst Covid-19 susceptible population-pools including cohorts from USA as well as India; the inflammatory cytokine Interleukin-1 beta (IL-1B) has immunotherapeutic potential for novel drug/biomarker-development in stratifying Covid-19 positive symptomatic population-subsets and borderline and/or asymptomatic subsets of both Covid-19 vaccinated and unvaccinated subgroups.
Moreover, the enigmatic array of Toll-like Receptors and Autophagy-cell death signaling cascade may be therapeutically targeted for demystifying the cellular/molecular/genetic basis of Covid-19 pathogenesis for eventual patient-friendly cost-effective Corvid-19 pandemic management globally.
One thing is clear, that the damage to the lungs is by an erratic and berserk immune response triggered by the COVID-19. virus. Is it possible to use steroids, like Triamcinolone, in higher dose rather than low dose prednisalone to stop this fatal and erratic immune response in selected patients who are progressing towards respiratory distress?
thank you, I think this is clear.
This is exactly why I do not want to compromise my lungs with a mask. In case I got Covid I want a strong respiratory system.
I read your article it’s fabulous. Some of my friends and relatives are really searching for this information. So I’m sharing these articles with them. So they too can get the benefit out of this. Thanks for sharing this article. Keep on sharing this kind of articles. Keep us more updated.
i like this article about How Severe COVID-19 Can Tragically Lead to Lung Failure and Death, For more than a year, the whole planet is suffering from the corona pandemic. It caused a lot of panic, fear, and anxiety.
People started to worry more about themselves, their families, and their beloved ones, which led them to take some more protective actions.
A lot of our daily routine has changed; staying home is all we can do now. And if we have to go out a lot of precautions must be taken.
We had really missed being in contact, hugging each other, shaking hands, and live freely.
However, it’s not done yet!
Like any virus, the Corona Virus or COVID-19 keeps mutating and changing in its genetic traits.
For example, a mutation had been revealed in the United Kingdom lately, causing a 70 % increase in the infection rate. While some scientists claim that also the death rate had increased by 30 %.
For instance, this mutation was also shown in several other countries, such as Brazil and South Africa, thanks for sharing this info