Genome Data Help Track Community Spread of COVID-19
Posted on by Dr. Francis Collins
Contact tracing, a term that’s been in the news lately, is a crucial tool for controlling the spread of SARS-CoV-2, the novel coronavirus that causes COVID-19. It depends on quick, efficient identification of an infected individual, followed by identification of all who’ve recently been in close contact with that person so the contacts can self-quarantine to break the chain of transmission.
Properly carried out, contact tracing can be extremely effective. It can also be extremely challenging when battling a stealth virus like SARS-CoV-2, especially when the virus is spreading rapidly.
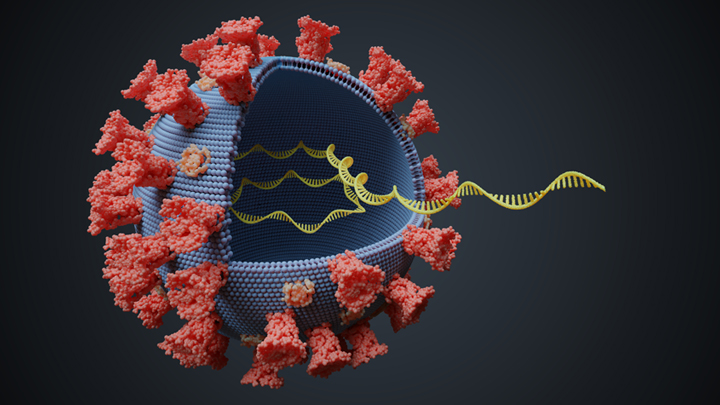
But there are some innovative ways to enhance contact tracing. In a new study, published in the journal Nature Medicine, researchers in Australia demonstrate one of them: assembling genomic data about the virus to assist contact tracing efforts. This so-called genomic surveillance builds on the idea that when the virus is passed from person to person over a few months, it can acquire random variations in the sequence of its genetic material. These unique variations serve as distinctive genomic “fingerprints.”
When COVID-19 starts circulating in a community, researchers can fingerprint the genomes of SARS-CoV-2 obtained from newly infected people. This timely information helps to tell whether that particular virus has been spreading locally for a while or has just arrived from another part of the world. It can also show where the viral subtype has been spreading through a community or, best of all, when it has stopped circulating.
The recent study was led by Vitali Sintchenko at the University of Sydney. His team worked in parallel with contact tracers at the Ministry of Health in New South Wales (NSW), Australia’s most populous state, to contain the initial SARS-CoV-2 outbreak from late January through March 2020.
The team performed genomic surveillance, using sequencing data obtained within about five days, to understand local transmission patterns. They also wanted to compare what they learned from genomic surveillance to predictions made by a sophisticated computer model of how the virus might spread amongst Australia’s approximately 24 million citizens.
Of the 1,617 known cases in Sydney over the three-month study period, researchers sequenced viral genomes from 209 (13 percent) of them. By comparing those sequences to others circulating overseas, they found a lot of sequence diversity, indicating that the novel coronavirus had been introduced to Sydney many times from many places all over the world.
They then used the sequencing data to better understand how the virus was spreading through the local community. Their analysis found that the 209 cases under study included 27 distinct genomic fingerprints. Based on the close similarity of their genomic fingerprints, a significant share of the COVID-19 cases appeared to have stemmed from the direct spread of the virus among people in specific places or facilities.
What was most striking was that the genomic evidence helped to provide information that contact tracers otherwise would have lacked. For instance, the genomic data allowed the researchers to identify previously unsuspected links between certain cases of COVID-19. It also helped to confirm other links that were otherwise unclear.
All told, researchers used the genomic evidence to cluster almost 40 percent of COVID-19 cases (81 of 209) for which the community-based data alone couldn’t identify a known contact source for the infection. That included 26 cases in which an individual who’d recently arrived in Australia from overseas spread the infection to others who hadn’t traveled. The genomic information also helped to identify likely sources in the community for another 15 locally acquired cases that weren’t known based on community data.
The researchers compared their genome surveillance data to SARS-CoV-2’s expected spread as modeled in a computer simulation based on travel to and from Australia over the time period in question. Because the study involved just 13 percent of all known COVID-19 cases in Sydney between late January through March, it’s not surprising that the genomic data presents an incomplete picture, detecting only a portion of the possible chains of transmission expected in the simulation model.
Nevertheless, the findings demonstrate the value of genomic data for tracking the virus and pinpointing exactly where in the community it is spreading. This can help to fill in important gaps in the community-based data that contact tracers often use. Even more exciting, by combining traditional contact tracing, genomic surveillance, and mathematical modeling with other emerging tools at our disposal, it may be possible to get a clearer picture of the movement of SARS-CoV-2 and put more targeted public health measures in place to slow and eventually stop its deadly spread.
Reference:
[1] Revealing COVID-19 transmission in Australia by SARS-CoV-2 genome sequencing and agent-based modeling. Rockett RJ, Arnott A, Lam C, et al. Nat Med. 2020 July 9. [Published online ahead of print]
Links:
Coronavirus (COVID-19) (NIH)
Vitali Sintchenko (University of Sydney, Australia)

The continuing COVID-19 infections in the Nursing Homes and other Elder Care facilities continues to spread. Has anyone tried to trace the path of these infections? The process that is being used to remove the path of the virus is not working. It would seem that the virus, as has been mentioned, travels through the air and/or by touching a surface that is contaminated.
Are all deliveries of supplies to these facilities inspected for the virus contamination? It can be on the delivered food supplies, mail, any other other delivered supplies, or brought in by anyone. I do not think just taking a temperature alone will detect the presence of the virus. The unbroken chain of the spreading virus continues to elude us. Finding the Root Causes of how the virus enters a Nursing Home facility and travels from it’s entry to infecting a person would be very challenging. Looking forward to the next New Year celebration, and people traveling to the celebration, just about 6months away, how will that be controlled?
“It would seem that the virus, as has been mentioned, travels through the air and/or by touching a surface that is contaminated.” Can you clarify the science behind surfaces as fomites for viral transmission? Are studies being replicated about viral viability on different surfaces? How much and what do we need to clean regarding food packaging?
If it is so contagious then why have we not been given or instructed what to do with used masks? This would be the biggest bio-hazard ever if it were true.
For the NIH Director, Dr Collins & Dr Fauci—you all are in the employ of Trump as long as he is President: at the time there is a safe & effective vaccine, you can engender public trust by quoting INDEPENDENT Research Scientists– if you can identify TRULY INDEPENDENT RESEARCH SCIENTISTS, maybe with the help of journalists.
I still do not see how this helps the primary purpose of contact tracing as the consequent isolation/quarantine has to be done very quickly to be of any use.
Found useful information …
“It would seem that the virus, as has been mentioned, travels through the air and/or by touching a surface that is contaminated.” Can you clarify the science behind surfaces as fomites for viral transmission? Are studies being replicated about viral viability on different surfaces? How much and what do we need to clean regarding food packaging?
Will it be possible to positively identify who infected you by using some genomic (or other scientific info) information carried by the covid virus? This will encourage people resisting vaccination to get vaccinated.