Study in Primates Finds Acquired Immunity Prevents COVID-19 Reinfections
Posted on by Dr. Francis Collins
There have been rare reports of people recovering from infection with SARS-CoV-2, the novel coronavirus that causes COVID-19, only to test positive a second time. Such results might be explained by reports that the virus can linger in our systems. Yet some important questions remain: Is it possible that people could beat this virus only to get reinfected a short time later? How long does immunity last after infection? And what can we expect about the duration of protection from a vaccine?
A recent study of rhesus macaques, which are among our close primate relatives, offers relevant insights into the first question. In a paper published in the journal Science, researchers found that after macaques recover from mild SARS-CoV-2 infection, they are protected from reinfection—at least for a while.
In work conducted in the lab of Chuan Qin, Peking Union Medical College, Beijing, China, six macaques were exposed to SARS-CoV-2. Following infection, the animals developed mild-to-moderate illness, including pneumonia and evidence of active infection in their respiratory and gastrointestinal tracts. Twenty-eight days later, when the macaques had cleared the infection and started recovering, four animals were re-exposed to the same strain of SARS-CoV-2. The other two served as controls, with researchers monitoring their continued recovery.
Qin’s team noted that after the second SARS-CoV-2 exposure, the four macaques developed a transient fever that had not been seen after their first infection. No other signs of reinfection were observed or detected in chest X-rays, and the animals tested negative for active virus over a two-week period.
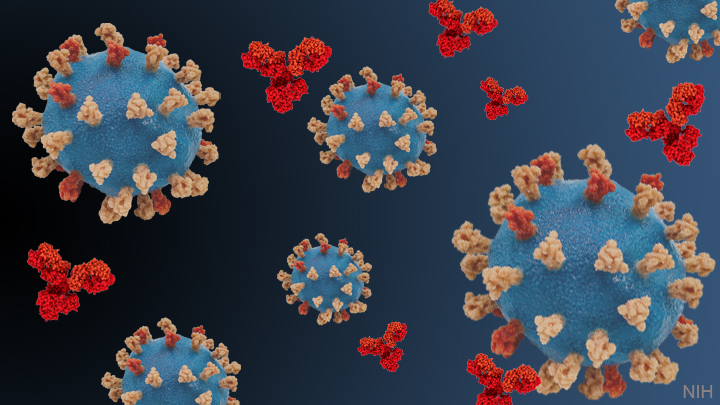
While more study is needed to understand details of the immune responses, researchers did detect a reassuring appearance of antibodies specific to the SARS-CoV-2 spike protein in the macaques over the course of the first infection. The spike protein is what the virus uses to attach to macaque and human cells before infecting them.
Of interest, levels of those neutralizing antibodies were even higher two weeks after the second viral challenge than they were two weeks after the initial exposure. However, researchers note that it remains unclear which factors specifically were responsible for the observed protection against reinfection, and apparently the first exposure was sufficient.
Since the second viral challenge took place just 28 days after the first infection, this study provides a rather limited window into broad landscape of SARS-CoV-2 infection and recovery. Consequently, it will be important to determine to what extent a first infection might afford protection over the course of months and even years. Also, because the macaques in this study developed only mild-to-moderate COVID-19, more research is needed to investigate what happens after recovery from more severe COVID-19.
Of course, macaques are not humans. Nevertheless, the findings lend hope that COVID-19 patients who develop acquired immunity may be at low risk for reinfection, at least in the short term. Additional studies are underway to track people who came down with COVID-19 in New York during March and April to see if any experience reinfection. By the end of this year, we should have better answers.
Reference:
[1] Primary exposure to SARS-CoV-2 protects against reinfection in rhesus macaques. Deng W, Bao L, Liu J, et al. Science. 2020 Jul 2. [Published online ahead of print].
Links:
Coronavirus (COVID-19) (NIH)
Qin Lab (Peking Union Medical College, Beijing, China)
Share this:
- Click to share on LinkedIn (Opens in new window)
- Click to share on Pinterest (Opens in new window)
- Click to share on Tumblr (Opens in new window)
- Click to share on Reddit (Opens in new window)
- Click to share on Telegram (Opens in new window)
- Click to share on WhatsApp (Opens in new window)
- Click to print (Opens in new window)

I am from India. In India a case of re-infection of this disease is detected as they say “Discharged patient tests COVID positive a second time.” One of our virologists, Dr. A Nandi says that the virus can spread even after 49 days of recovery from the virus. This means that even if the patient himself/herself doesn’t get infected, he/she is capable of spreading the virus even after 49 days. But, cases of re-infection are very low for this disease, at least till now. Needs further study for this!
In this context, let me request something! As the airborne transmission of this virus is becoming dominant, I think you can post something on this matter.
Scientifically stimulating study dissecting pathogenesis and replication alongwith immuno-virulence/reinfection statuses ranging from symptomatic mild to moderate Covid-19 positivity in animal models of research, primarily rhesus macaques/primates!
I wish to add that gender male vs female and strain/species-specific subgroup analysis by relevant adjustment of covariates/confounders in a multicentric primate-model-based Covid-19/SARS-2 mild-to-moderate sensitivity/reinfection/immunogenecity/relapse rates with statistical analyses involving larger sample size based data-sets and subsequent stratification of case-numbers viz. Covid-19 positive mild-infection primates vs moderate-infection primates using Bonferroni’s corrections fro multiple comparisons would yield novel critical research insights in translational medicine field.
Further, stratification of mild vs moderate infection status primates of female gender using age, parity/pregnancy status (non-pregnant vs pregnant Rhesus macaques) would further aid in designing future patient-centric Covid-19 research studies for further Covid-19-SARS2-infection and transmission at the maternal-fetal interface. Such studies would be useful for designing eventual animal research models of Covid-19 genetic susceptibility; replicative genetic association case-control studies may provide further insights for long-term management of Covid-19 infection globally.
Overall, an elegant study with innovative insights for developing cost-effective public health research models for diminishing the disproportionate share of morbidity and mortality associated with Covid-19 in ethnically distinct populations; moreover, the current study has tremendous relevance in future design of pharmacological scaffolds, novel drugs and predictive biomarkers for Covid-19 susceptibility.
Hey Nice Blog!! Thanks For Sharing!!!
I had a mild bout of COVID on March 14 and then a more severe bout of it on March 29 – April 12. I tested negative for the virus with a PCR test (throat swab – non FDA approved test) on March 31. I tested positive for IgG antibodies (LabCorp) on June 6. I wonder if I had one infection that started on March 13 and resurrected later in March or if I had 2 infections, the second one being more severe.
It baffles me that attention is paid to a 6 monkey study over a mere month, while a King’s College longitudinal study of 65 patients that tracked the decline of their antibodies to SARS-CoV-2 over 94 days is ignored. The later seems to be a more relevant picture of what is likely to happen in humans.
It doesn’t baffle me that they are paying attention to this study at all. IgG and IgM may very well be observed to dissipate a relatively short time after acute infection, but that is not all our human immune systems have in their arsenals. It appears our T cells may also afford immunity even when IgG and IgM have faded. So this study is absolutely worthwhile in the scheme of things. No doubt, the study is extending and the primates will be exposed again at a later date, and again and again. Of course I may be wrong, but I suspect focusing solely on IgG and IgM levels is both narrow and short-sighted. At this point, I don’t believe there are ANY documented cases of actual proven re-infection in humans. It doesn’t mean there won’t be, but the longer we go without seeing actual evidence of this, the better our chances are that humans are acquirIng lasting immunity-whether it’s a year or a lifetime remains to be seen as time unfolds.
The goal here is to try, with the help of modelling, to unpack the processes by which Covid-19 epidemics can be controlled – even ended.
In fact, it is often unclear whether the numbers will tail off towards zero, will surge back up, or will simply hover around some baseline level.
If antibodies don’t last long then either will the vaccine.
Scientifically stimulating study dissecting parthenogenesis and replication along with immune-virulence/reinfection statuses ranging from symptomatic mild to moderate Covid-19 positivity in animal models of research, primarily rhesus macaques/primates!
I wish to add that gender male vs female and strain/species-specific subgroup analysis by relevant adjustment of covariates/confounders in a multicentric primate-model-based Covid-19/SARS-2 mild-to-moderate sensitivity/reinfection/immunogenecity/relapse rates with statistical analyses involving larger sample size based data-sets and subsequent stratification of case-numbers viz. Covid-19 positive mild-infection primates vs moderate-infection primates using Bonferroni’s corrections fro multiple comparisons would yield novel critical research insights in translational medicine field.
Further, stratification of mild vs moderate infection status primates of female gender using age, parity/pregnancy status (non-pregnant vs pregnant Rhesus macaques) would further aid in designing future patient-centric Covid-19 research studies for further Covid-19-SARS2-infection and transmission at the maternal-fetal interface. Such studies would be useful for designing eventual animal research models of Covid-19 genetic susceptibility; replicative genetic association case-control studies may provide further insights for long-term management of Covid-19 infection globally.
Overall, an elegant study with innovative insights for developing cost-effective public health research models for diminishing the disproportionate share of morbidity and mortality associated with Covid-19 in ethnically distinct populations; moreover, the current study has tremendous relevance in future design of pharmacological scaffolds, novel drugs and predictive biomarkers for Covid-19 susceptibility.
My husband was positive in July with no symptoms, then tested negative x2, then on sept 4 tested positive again with no symptoms. What does this mean.? Are we being lied to, does one really develop any immunity to this disease?
I first tested positive at the end of July. Symptoms were mainly respiratory and moderate. After 14 days symptoms had subsided and I returned to work. I was then positive a second time at the first of September. This time I had loss of taste and smell and had GI symptoms. Symptoms lasted approximately 7-9 days. I have now tested positive a third time November 4th. This time symptoms are headache, dizziness, nausea, fatigue. How do I continue to get reinfected? How do you prevent a fourth time? Please advise.