Genes, Blood Type Tied to Risk of Severe COVID-19
Posted on by Dr. Francis Collins
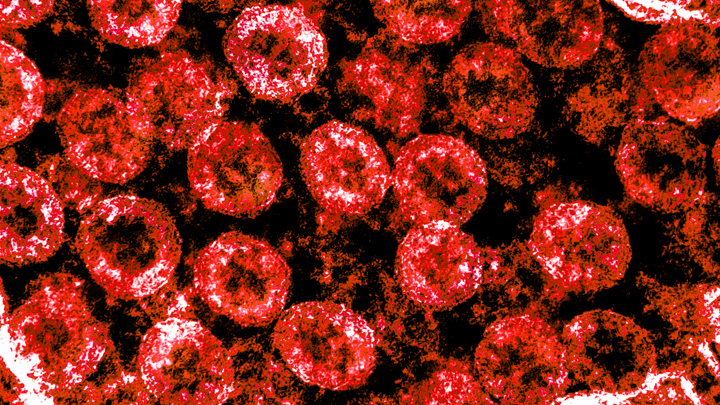
Credit: National Institute of Allergy and Infectious Diseases, NIH
Many people who contract COVID-19 have only a mild illness, or sometimes no symptoms at all. But others develop respiratory failure that requires oxygen support or even a ventilator to help them recover [1]. It’s clear that this happens more often in men than in women, as well as in people who are older or who have chronic health conditions. But why does respiratory failure also sometimes occur in people who are young and seemingly healthy?
A new study suggests that part of the answer to this question may be found in the genes that each one of us carries [2]. While more research is needed to pinpoint the precise underlying genes and mechanisms responsible, a recent genome-wide association (GWAS) study, just published in the New England Journal of Medicine, finds that gene variants in two regions of the human genome are associated with severe COVID-19 and correspondingly carry a greater risk of COVID-19-related death.
The two stretches of DNA implicated as harboring risks for severe COVID-19 are known to carry some intriguing genes, including one that determines blood type and others that play various roles in the immune system. In fact, the findings suggest that people with blood type A face a 50 percent greater risk of needing oxygen support or a ventilator should they become infected with the novel coronavirus. In contrast, people with blood type O appear to have about a 50 percent reduced risk of severe COVID-19.
These new findings—the first to identify statistically significant susceptibility genes for the severity of COVID-19—come from a large research effort led by Andre Franke, a scientist at Christian-Albrecht-University, Kiel, Germany, along with Tom Karlsen, Oslo University Hospital Rikshospitalet, Norway. Their study included 1,980 people undergoing treatment for severe COVID-19 and respiratory failure at seven medical centers in Italy and Spain.
In search of gene variants that might play a role in the severe illness, the team analyzed patient genome data for more than 8.5 million so-called single-nucleotide polymorphisms, or SNPs. The vast majority of these single “letter” nucleotide substitutions found all across the genome are of no health significance, but they can help to pinpoint the locations of gene variants that turn up more often in association with particular traits or conditions—in this case, COVID-19-related respiratory failure. To find them, the researchers compared SNPs in people with severe COVID-19 to those in more than 1,200 healthy blood donors from the same population groups.
The analysis identified two places that turned up significantly more often in the individuals with severe COVID-19 than in the healthy folks. One of them is found on chromosome 3 and covers a cluster of six genes with potentially relevant functions. For instance, this portion of the genome encodes a transporter protein known to interact with angiotensin converting enzyme 2 (ACE2), the surface receptor that allows the novel coronavirus that causes COVID-19, SARS-CoV-2, to bind to and infect human cells. It also encodes a collection of chemokine receptors, which play a role in the immune response in the airways of our lungs.
The other association signal popped up on chromosome 9, right over the area of the genome that determines blood type. Whether you are classified as an A, B, AB, or O blood type, depends on how your genes instruct your blood cells to produce (or not produce) a certain set of proteins. The researchers did find evidence suggesting a relationship between blood type and COVID-19 risk. They noted that this area also includes a genetic variant associated with increased levels of interleukin-6, which plays a role in inflammation and may have implications for COVID-19 as well.
These findings, completed in two months under very difficult clinical conditions, clearly warrant further study to understand the implications more fully. Indeed, Franke, Karlsen, and many of their colleagues are part of the COVID-19 Host Genetics Initiative, an ongoing international collaborative effort to learn the genetic determinants of COVID-19 susceptibility, severity, and outcomes. Some NIH research groups are taking part in the initiative, and they recently launched a study to look for informative gene variants in 5,000 COVID-19 patients in the United States and Canada.
The hope is that these and other findings yet to come will point the way to a more thorough understanding of the biology of COVID-19. They also suggest that a genetic test and a person’s blood type might provide useful tools for identifying those who may be at greater risk of serious illness.
References:
[1] Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Wu Z, McGoogan JM, et. al. 2020 Feb 24. [published online ahead of print]
[2] Genomewide association study of severe Covid-19 with respiratory failure. Ellinghaus D, Degenhardt F, et. a. NEJM. June 17, 2020.
Links:
The COVID-19 Host Genetics Initiative
Andre Franke (Christian-Albrechts-University of Kiel, Germany)
Tom Karlsen (Oslo University Hospital Rikshospitalet, Norway)

Why are all these people asking for medical advice in the comment section of this article??!?!?!?!?!?!
Many are probably desperate and cannot afford the US health care system. Sad but probably true.
Seems to make sense, well done, looking forward to more news on this subject
We are interested in your studies regarding the severity of the covid19 virus on individuals with type A and type O negative blood since this relates to my husband and me.
Me Too! I want to know how many people who are Rh Negative have had Covid-19 and how many people who were Rh Negative have died from Covid-19 too!
I am disappointed that few are paying much attention to Rh factor in these statements. Within the primary research that the above information references is a further reference that essentially posits that Rh factor is a dominant indicator of risk. You can find this information here: Zietz M, Tatonetti NP. Testing the association between blood type and COVID-19 infection, intubation, and death. April 11, 2020 (https://www.medrxiv.org/content/10.1101/2020.04.08.20058073v1. opens in new tab).
Me too! Please let me know if you find any information on RH negative in regards to Covid.
I have RH-A and my daughter too. The rest of the family in my home do not. There’s 8 people in our home, and we’re scared to death of where are we supposed to go if we get this horrific virus? I also have underlying health issues, which in itself is terrifying. My husband’s side has a family reunion this weekend and I have to ask, where do I go to quarantine myself when they get back??? And for how long??? I’m trying to get as much research on my blood type as possible.
Quite interesting and makes sense.
My blood type is 0-, rh- . I heard that people who’s rh- are resistant to certain viruses. Is there any truth to that?
Has there been an answer to this question?
This virus has so many facets, with the blood clotting one being among the most frightening. Hopefully what we learn will help us when we experience the next pandemics, as it is difficult to imagine us being able to convince people with the custom of eating wild animals to give it up.
My father in law is 94. He lives in a nursing home. He had 2 positive tests then a negative result came today. He is B+ blood type.
Was he a mild case?
Brenda S…how severe was his COVID? My Son is blood Type B+ Too
What about AB blood groups are they at risk?
I have AB negative blood type. It is the rarest blood type, I am more likely to get sick if I contract the coronavirus?
I have been diligently following and have not recorded one case with AB negative blood yet. I suspect it is like Norovirus… The mechanism that the virus uses to attach to cells are incompatible with our blood type.
Does the Rh factor make a difference also? Is A+ at a higher risk than A- blood type?
I have Type O blood (read the NEJM article) My question is about how likely it is for this blood type to be an asymptomatic carrier, possibly endangering others more than oneself.
My Blood Group is AB+ve ,four days back I got cold and fever after three days symptoms Normal. I don’t know what’s happened
As I read this, the denominator of the ratio of type O victims of Covid-19 would not include the people who had very mild, asymptomatic cases and therefore never sought testing. In other words, the percentage benefit to type O people may be bigger than the numbers suggest. Is this a legitimate observation?
if AB have no antibodies, how do vaccines work and are there the gene and blood tests available now?
Im am A- Rh negative I have never had a virus ever in my life I have never had the flu and don’t get any Vaccines. I avoid modern Medicine if at all possible. I have been around a positive covid Patient and never contracted the virus I tested negative.
Is it possible that there are some folks that could have a immunity?
Excellent post. I will share this blog to my social profile …
Very interesting. I am O+ and very rarely get sick at all. I have not had a cold in well over ten years and have been exposed multiple times a year. I am a nurse and work in LTC. I will be interested to see what further information comes from this research. Thank you for publishing this information.
Why O Negative is less likely to ever die from it because they don’t have the red proteins on the blood cells. so the 50% chance of the 00 blood type not getting it or the higher risk of not getting severe cases of it is the negative type not the O positive and O positive is still has a rhesus monkey bloodgene cell’s contain proteins on the red blood cells that causes them to be affected by it due to the fact that the proteins on the cells is what the coronavirus attacks I’ve been trying to tell CDC this ever since the beginning of this that as I believe I had it back in January nobody listens to me but what the hell ever I think I’ve been a perfect candidate for the antibodies on it from day one but nobody’s listening to me
Anyways I did talk to text on this so if it’s a little messed up I’m sure you can figure it out
o+ here, believe I had Covid-19 in Early January. Tested Positive for Antibodies May 8. Been Donating Convalescent Covid Plasma twice a week since End of May. We are Hearty, We can make a difference and Save lives. Be Proactive Help where you can. Peace!
Where can I do that at?
In San Diego, the San Diego Blood Bank is testing for antibody’s through the end of July, and if you have them they will accept the covid plasma donations. I’d check with your local blood bank. It may be a National initiative as I understood they were required to report the results of all the tests positive or negative.
Type A and still healthy as a horse. Not doing anything differently except going to the store less. Wear your mask and wash your hands!
I am B+ I rarely get sick and when I do it doesn’t last very long In February I had symptoms of a cold/flu that lasted less time than any other time in my life, only two days. I went to work Friday feeling fine, I woke up Saturday feeling awful thinking this was going to last for a while but I started feeling better Sunday evening and Monday I was completely fine.
For me I notice by me being O positive the people that lived with me are all tested positive for covid but my 2 test came back negative I had no symptoms but sinuses migraine and they were really sick with 102.4 fever,diarrhea and throwing up a lot, but I asked the doctor’s office how can everyone around me be sick and positive and I’m not? Still waiting for my answer.
The same thing happened to me with my family. My family tested positive and I tested neg twice and no antibodies with strange symptoms. I have O- Neg blood
I’m O+ and my hubby and son tested positive on Monday while both of my test are negative but Nevertheless as others have stated with my blood type I do have a severe headache a scratchy throat, slight congestion in my chest, body aches, no fatigue, no loss of smell or taste overall I’m doing good!
Stay safe and healthy
Hi, I’m AB-negative and a member of an online rhesus negative group. It’s world-wide group, and we talk regularly. I will inform you that the question has arisen of whether any of us have caught it? And the answer put up by practically everyone was a huge NO.
These are great comments. All the information helps in learning more about this virus!