Genes, Blood Type Tied to Risk of Severe COVID-19
Posted on by Dr. Francis Collins
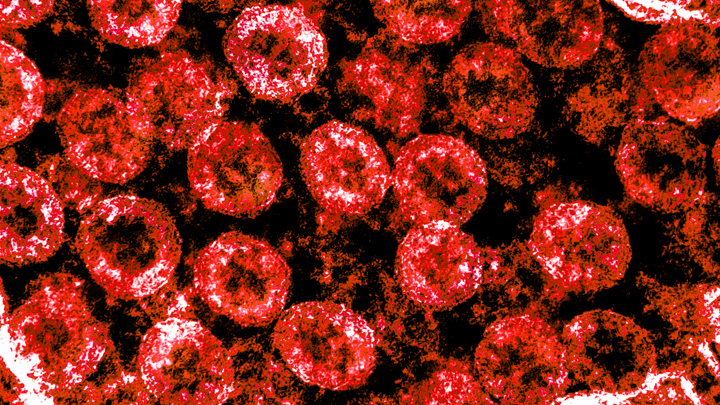
Credit: National Institute of Allergy and Infectious Diseases, NIH
Many people who contract COVID-19 have only a mild illness, or sometimes no symptoms at all. But others develop respiratory failure that requires oxygen support or even a ventilator to help them recover [1]. It’s clear that this happens more often in men than in women, as well as in people who are older or who have chronic health conditions. But why does respiratory failure also sometimes occur in people who are young and seemingly healthy?
A new study suggests that part of the answer to this question may be found in the genes that each one of us carries [2]. While more research is needed to pinpoint the precise underlying genes and mechanisms responsible, a recent genome-wide association (GWAS) study, just published in the New England Journal of Medicine, finds that gene variants in two regions of the human genome are associated with severe COVID-19 and correspondingly carry a greater risk of COVID-19-related death.
The two stretches of DNA implicated as harboring risks for severe COVID-19 are known to carry some intriguing genes, including one that determines blood type and others that play various roles in the immune system. In fact, the findings suggest that people with blood type A face a 50 percent greater risk of needing oxygen support or a ventilator should they become infected with the novel coronavirus. In contrast, people with blood type O appear to have about a 50 percent reduced risk of severe COVID-19.
These new findings—the first to identify statistically significant susceptibility genes for the severity of COVID-19—come from a large research effort led by Andre Franke, a scientist at Christian-Albrecht-University, Kiel, Germany, along with Tom Karlsen, Oslo University Hospital Rikshospitalet, Norway. Their study included 1,980 people undergoing treatment for severe COVID-19 and respiratory failure at seven medical centers in Italy and Spain.
In search of gene variants that might play a role in the severe illness, the team analyzed patient genome data for more than 8.5 million so-called single-nucleotide polymorphisms, or SNPs. The vast majority of these single “letter” nucleotide substitutions found all across the genome are of no health significance, but they can help to pinpoint the locations of gene variants that turn up more often in association with particular traits or conditions—in this case, COVID-19-related respiratory failure. To find them, the researchers compared SNPs in people with severe COVID-19 to those in more than 1,200 healthy blood donors from the same population groups.
The analysis identified two places that turned up significantly more often in the individuals with severe COVID-19 than in the healthy folks. One of them is found on chromosome 3 and covers a cluster of six genes with potentially relevant functions. For instance, this portion of the genome encodes a transporter protein known to interact with angiotensin converting enzyme 2 (ACE2), the surface receptor that allows the novel coronavirus that causes COVID-19, SARS-CoV-2, to bind to and infect human cells. It also encodes a collection of chemokine receptors, which play a role in the immune response in the airways of our lungs.
The other association signal popped up on chromosome 9, right over the area of the genome that determines blood type. Whether you are classified as an A, B, AB, or O blood type, depends on how your genes instruct your blood cells to produce (or not produce) a certain set of proteins. The researchers did find evidence suggesting a relationship between blood type and COVID-19 risk. They noted that this area also includes a genetic variant associated with increased levels of interleukin-6, which plays a role in inflammation and may have implications for COVID-19 as well.
These findings, completed in two months under very difficult clinical conditions, clearly warrant further study to understand the implications more fully. Indeed, Franke, Karlsen, and many of their colleagues are part of the COVID-19 Host Genetics Initiative, an ongoing international collaborative effort to learn the genetic determinants of COVID-19 susceptibility, severity, and outcomes. Some NIH research groups are taking part in the initiative, and they recently launched a study to look for informative gene variants in 5,000 COVID-19 patients in the United States and Canada.
The hope is that these and other findings yet to come will point the way to a more thorough understanding of the biology of COVID-19. They also suggest that a genetic test and a person’s blood type might provide useful tools for identifying those who may be at greater risk of serious illness.
References:
[1] Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: Summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. Wu Z, McGoogan JM, et. al. 2020 Feb 24. [published online ahead of print]
[2] Genomewide association study of severe Covid-19 with respiratory failure. Ellinghaus D, Degenhardt F, et. a. NEJM. June 17, 2020.
Links:
The COVID-19 Host Genetics Initiative
Andre Franke (Christian-Albrechts-University of Kiel, Germany)
Tom Karlsen (Oslo University Hospital Rikshospitalet, Norway)

There are 5 members of our household, myself, my wife and 3 adult daughers. Covid went through our house. Everyone had strong symtoms but me. I’m O+
I was exposed to both my teenagers over a period of time. They both tested positive for covid and I tested negative twice. I did get some strange symptoms at the time but continued testing neg for virus and tested neg for antibodies. I have O- Neg blood. Very bizarre and perplexing for me
Me too. Only way I figure I avoided catching Covid-19 & any of it’s variants was fully vaccinated…usual precautions and O-blood type !!!
My whole family of seven were exposed to COVID recently. My wife is O- my kids and I are O+ (3 sons & 2 daughters). My oldest daughter (18) & I still have tested negative multiple times, my youngest daughter (6) tested positive but is asymptomatic. My wife and kids’ symptoms were similar to sinus infection very mild symptoms.
I was in the ICU 13 months ago with kidney problems due to a bad infection. After I had been there for 12 days, they wanted to do a surgical procedure to remove a kidney stone, and the night before, they did a rapid covid test.
I had zero symptoms of covid, but they said it was a regular practice before a surgical procedure.
Shockingly, the results came back positive. Given the fact that my blood pressure was extremely low and my kidneys were weak, they moved me to the Covid isolation floor. (FYI. That’s a scary place!) They expected I would need a ventilator relatively quickly. But, to everyone’s amazement, I remained 100% symptom-free.
They kept me there for a day and a half and then sent me home to self-quarantine. Four days after testing positive, I lost my sense of taste and smell. Two days later, I was perfectly fine and spent the rest of the quarantine bored to tears.
Later at a follow-up visit, my doctor told me that statistics were showing Covid is blood type-specific. People with Type-A were much more likely to develop acute respiratory problems than people who have Type-O. My blood type is O-, and afterward, they asked me if I would be willing to sign up to donate blood for the purpose of convalescent blood transfusion therapy.
The antibody tests have consistently shown my blood has a high level of antibodies. I agreed and am currently on standby with Baylor Scott & White and the Carter Blood Center to donate blood.
Royal blood my friend,Royal blood.
Awwwwn praise the lord I am O as well my momma told me I have more white blood cells then red which means my body has a strong Defence in fighting off those monsters.
I have been in a household of 4 with 3 positive results of COVID . Me being the fourth in the house hold and have a lung disease and am very suspectable to hospitalization because of my lung disease. I have blood type O+ and have not caught covid to everyones amazement. I got some symptoms of COVID ,taste,aching,headache , fatigue, breathing troubles and all were sure including my own doctor that I had contracted COVID but I had previously had 2 rapid tests done both negative and when I had gotten even more symptoms and took the lab send off test, received my results after 48 hours and it came back negative! I give first and foremost the glory to God! And thank him for blessing me with O+ blood type as COVID would have surely taken my life. Praise and Glory to God! I am praying for each and every one who faces this awful disease for God to heal them all and bring each through it! Stay healthy to all and stay covered under the precious blood of Jesus!
My wife and I (both A+ blood type and both 70 yrs old) tested positive in early July 2020. She spent 8 days, and I spent 11 days in hospital. My O2 was at 77% when I went by ambulance. Really did not think I was going to make it out. Came home with 02 for 2 months 24/7. Fast forward to Jan 2021. Got 1st Moderna shot. 12 hrs later: nausea, teeth chattering chills, hot sweats, and every joint and muscle ached. Could not get out of bed next morning. Took 800 mg Ibuprofen and was able to slowly get up 45 min later. By 3rd day I was back to normal but extremely fatigued. 2nd shot on Feb 14th. Same symptoms but much, much milder. Wife went thru same but much less severe on all fronts.
Was wondering if PF4 blood factor has any protection against severe Covid. I have that and thus far no covid and no reaction to vaccine. I know I can’t get Malaria with that blood factor. Just curious.
On Thanksgiving Day I had a runny nose. I worked the next day and was off the weekend. I thought I had a sinus infection so I took medication for those symptoms. Only ran a low grade temp on Friday of 99 degrees. I worked with no symptoms Monday and Tuesday and had routine heck at work where I found out I had COVID. I was in disbelief. My symptoms were mild. I’m a 48-year-old woman. My husband’s symptoms were similar and our daughter did not contract it.
What are the blood types?
Has there been any research done on whether increased severity of Covid-19 symptoms in blood type As is associated with whether or not the individual is homozygous or heterozygous? Are homozygous type A blood type individuals at higher risk than heterozygous type As?
I’m type O- and lost my entire sense of taste and smell in mid December 2019. I also had a week long spate of gastro-intestinal symptoms and strange dreams (no fever or SpO2 issues). I thought it was due to the CBD isolate I was using for diabetic nerve pan in my feet (I’m 78 and have diabetes, heart failure, and cancer) but am otherwise in good physical condition for my age and underlying co-morbidities (6′ – 3″, 205 lbs, and can bench press 175 lbs. (50 reps)). I’m just now able to smell (~60%) and taste (~80%), but both are off and on. I’m fully immunized with the Moderna Vaccine as of 03/26/2021, and believe the vaccine improved my 1+ year “long covid” symptoms. Who may know? My entire family have type O- blood and have experienced similar loss of taste and smell episodes but no severe Covid-19 illness! I concluded by March 2020 that I was blessed with Type O-Neg Blood! The foregoing is for what it is worth to any readers.
I contracted covid 19 in Dec 2020. I spent 9 weeks in the hospital. 45 days on a ventilator. I am type A positive. 7 months later I am still on oxygen. I have been in an extensive rehab program for the last 4 months. My specialists say I am a miracle. I was told by ICU intensivist that it might take a year to heal my lungs. I am in my 40’s.
Wow that is crazy. Hope you get better soon.
My husband has type A blood and he was able to treat his Covid infection at home, all he had was a high fever 102 -104 F, a bad productive cough with loss of taste and smell. I have O- blood and I was stuck in the hospital for 8 days during my Covid infection with pneumonia in both lungs, high fevers 103 -104 F and was coughing up blood as my D-dimer levels were over 1000 and I was giving a blood thinner to bring it down. I needed high levels of oxygen to fight off the extreme hypoxemia I had. Thankfully I didn’t need to be intubated, though the doctors were preparing to if my levels didn’t start going up. Was given Remdesivir which caused my ALT and AST to go high for a while. Not sure if this makes a difference but I do have co-morbidities of Rheumatoid Arthritis and Celiac disease. The thing that is interesting is that I drove both myself and my husband to the ED because my husband had a really bad productive cough and high fevers that wouldn’t go down even after taking a fever reducer. I, at the time only had a high level of fatigue and kept falling asleep, later found to be a %SpO2 of 70, while waiting in the waiting room with him to get seen and a high fever that wouldn’t go down even with a fever reducer and no sense of taste or smell. The only good thing out of it was that I lost 12 lbs. due to not wanting to eat the hospital’s food,they really need to improve their gluten- free menu.
Well I am O Negative and Rh Negative but I have COX-26 as a recessive gene causing genetic deafness in my Family Tree…. Then I have diabetes type-2, hypertension, IBS…. I have B.A. in double-majors of Biology and Chemistry from Gallaudet University…. Now I am nearly 70 years old but retired….
I received a first dose of Pfizer vaccine on March 25 and a second dose on April 15…. Since March 12 2020, I am quarantined at my home, then I really comply with CDC guidelines as I practice in preventive hygiene like using 6 feet distance, washing hands with soap & water and hand sanitizer as I always wear masks inside in the apartment complex and outside in preventive and protective measures to stay well and alive but positive.
Have 0- type am 80 years old. Stay home most of time but wear masks when I leave. Am overweight but no serious illnesses. I’ve never had any symptoms did test twice negative. Had 1st Moderna shot in February and 15 days later had Moderna arm- huge rash where shot was given. 2nd day after 2nd shot felt horrible. Could barely move for 24 hours and since then I’m good, at least free from Covid but still careful.
I am O negative blood type, I have been twice (June 2020 and November 2020) in contact with people who tested positive for Covid and the person in November died 10 days after he tested positive, and thank God I tested negative. In Feb 2021 I got a nasty cold, excessive coughing, felt horrible and even a bitl short of breath, I went to test and they said negative. I tookk a course of Zpak (antibiotics) and got better. I am still on the fence about the vaccine. I use a mask and try to stay away from large crowds. I am 57 femaile with no underlying medical condition.
Royal Blood!
I am 63 and O+. My wife has had covid twice, my 92 year old mother has had it and was never ill. I drove my wife around all day (she travels for work) for almost 2 weeks in February because she was so weak. There was no test for covid then, she found out she had antibodies in April that proved she had had it in February. I have been in contact and then tested negative at least 7 times. I took the Moderna shot twice with no effect whatsoever either time. I knew several people who have died and others who became seriously ill. I don’t feel bulletproof at all against this awful thing, but, I have rarely been sick in my life and have had the flu only once that I know of, and now almost constant exposure to covid and nothing. In my mind, there has to be something about blood type and immune system strength. I give thanks to God that I have not fallen ill and pray for the families that have been struck by this mysterious monster.
My wife is 69 and I am 73. She has O pos and I am O neg. we both tested positive for covid on14 Dec 2020. She had a loss of taste and feeling overall miserable. No breathing problems. I had what seemed like a sinus infection. I walk 3 miles a day and never stopped my routine. Temps in 20 and 30 s here. No breathing problems, or headaches or fever. It took her longer to get better than me. We both got the Moderna vaccine in March and second in April. I got an overnight fever after each shot. Wife lesser affected by shots. We traveled all over last year and saw the grandkids numerous times. We never stopped our routine. Except for the 10 day quarantine. We are at healthy weights, wife has chronic pancreatitis and R A. She is taking Plaqenil for that. Both of us have had heart attacks in the past. Each of us have a single stent. My attack was 15 years ago and hers was 6 years ago.
What about type B, + and -?
Had Pfizer vaccine 12 days ago and coughed up phlegm for 11 days later. Am feeling some better but concerned that my ab positive blood type and having tested positive back in June 2020 might have been a factor?
I had a slightly wet cough Christmas 2020. I’m A+. I tested positive for Covid-19 two days after Christmas. My symptoms never got any worse than that slightly wet cough.
MIL had Covid May 2020 recovered enough to return to nursing home 2 weeks later returned to ICU they couldn’t keep fluids off her lungs. She died June 10th 2020. July 2020 my husband type A- had covid was sick solid 5 weeks, he still has some smell and taste loss. My 80 yr old mom (type 0+) and I (A+) both had mild symptoms at that time but were unable to get tested until 3 weeks after exposure. I tested negative at that time. Fast forward Jan 2021 I had a scratch dry throat and felt tired. Tested positive my symptoms we were mild and lasted about 5 days . My mom had mild symptoms for a few days and on Feb 2 nd tested negative. 6 weeks later I still tested positive. In Aug 2021 mom had a UTI and was put on Antibiotics a few days late she exhibited cold symptoms. Fever, chills, cough, runny nose. But due to the antibiotic side effects making her feel terrible and everything taste terrible. She refused to get tested or see a doctor. 6 weeks later at her req ck up she tested positive for antibodies.
May I ask what the broader response for this research has been amongst the scientific/medical communities? We continue to treat everything as a nail and there is only one hammer in slowing the spread and defeating the inherent risk of CV19 in general which is vaccination.
Please do not take this post as an “anti-vaccination” position, I am all for vaccinating the most vulnerable – A blood types – according to the above research. My logic here being a Type 1 diabetic with Type O- blood being exposed – severely in some cases – to the CV19 virus, not having contracted it, and not having antibodies for it, wouldn’t I be risking other’s safety if I intentionally vaccinate with a viral load then continue my everyday life?
In other words if my metabolic and health profile (low inflammation) coupled with Type O- blood naturally defeats SARS-CoV-2 binding to my cells, am I already protecting others by maintaining my overall health? More importantly, if I choose to vaccinate and bind those to my Type O- cells, wouldn’t I risk infecting others for a 2-3 week period? Or create a pattern where I pose a risk of additional mutation spread and intentional inflammation within my own body?
These are worthwhile studies to share more broadly again with scientific evidence that demonstrates who more strategically should/could be vaccinated. If it poses a risk to Type O- individuals to contract or increase spread, we need to incorporate that into the solution direction as at a minimum a discussion for frontline healthcare workers to consider.
Thanks for the review and continuing the research on this important topic!
Excellent question. It is very concerning how little curiosity has been shown about this angle.
I am 0+ and have not contracted covid thus far. I tested twice. I have had Moderna 2x and the same for booster. Was exposed on Christmas day but still ok 12 days later. I see from the posts that other 0 types report good outcomes except for one. Very interesting and I look forward and hopeful to following this research.
I think we will come to find that blood type affects one’s reaction to Covid. I am deeply disappointed that this is not being studied in detail.