Personalized Cancer Vaccine Enters Human Trials
Posted on by Dr. Francis Collins
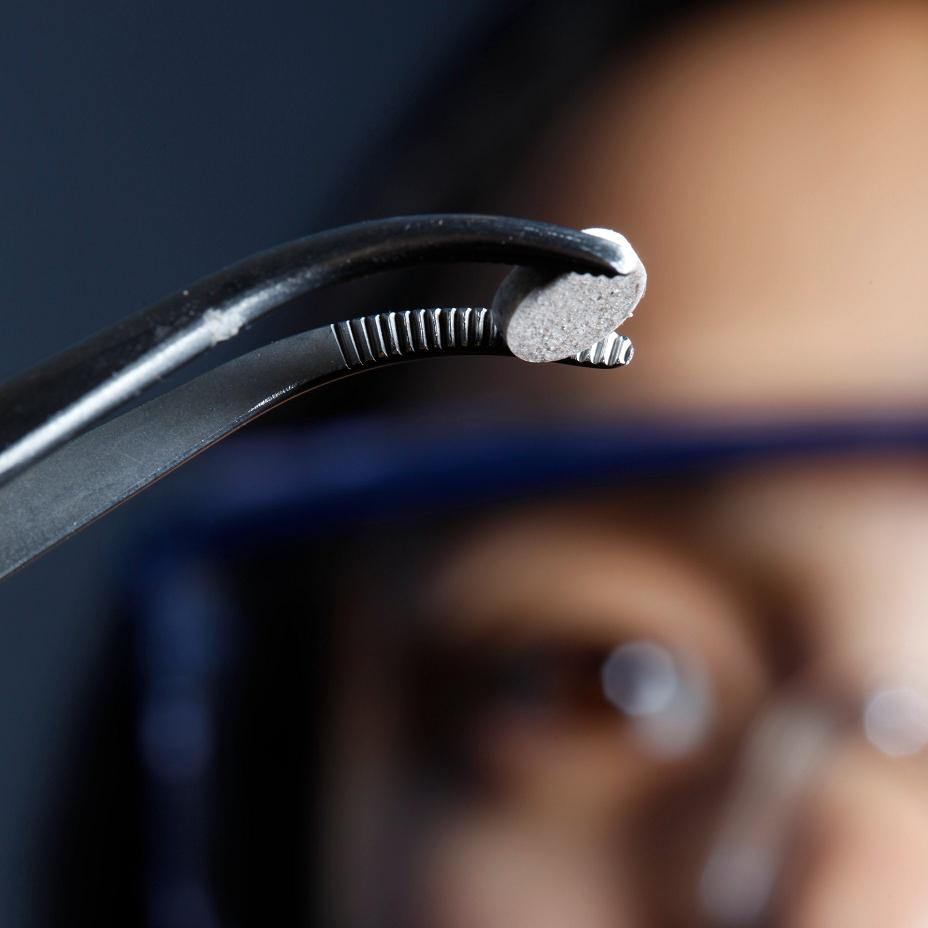
Caption: The new melanoma vaccine, which is implanted beneath the skin, is now being tested in human trials.
Credit: Wyss Institute and Amos Chan
This aspirin-sized disk is the first therapeutic cancer vaccine implanted beneath the skin [1]. We know it can eradicate melanoma in mice—the deadliest form of skin cancer—with impressive efficacy [2]. Now, it’s being tested in human trials.
First, a few words on vaccines. Usually, when we think of vaccines, we think of preventive vaccines, and most commonly the goal is to provide immunity to an infectious agent. The smallpox vaccine is a classic example. So is vaccination against the human papilloma virus (HPV)—a powerful way to prevent cervical cancer. In contrast, the implanted cancer vaccines we’re looking at today are therapeutic: they’re given to patients who have already been diagnosed with cancer. Once administered, though, they behave like traditional vaccines—by teaching the immune system how to seek out and destroy a target—in this case, a tumor.
Therapeutic cancer vaccines are a new, and hot, research area. A couple of cancer vaccines have already been approved by the FDA. However, producing these vaccines is typically a cumbersome, time-consuming, and expensive process. First, immune cells are taken from a patient. The cells are modified and reprogramed in the lab, and then they are injected back into the patient. In the vaccines approved to date, this elaborate production line has extended patient life—but only slightly. And so, some researchers began to look for a simpler, and perhaps more effective, way to make therapeutic cancer vaccines. About four years ago, an NIH-funded, multidisciplinary team based in Boston and Cambridge came up with an approach that would modify and reprogram patients’ immune cells—inside the body, not in a lab.
The team first developed a porous polymer implant, made from the same material as biodegradable sutures and meshes. Then they infused the disk with a collection of three immune stimulants that recruit the immune cells, activate them, and imprint them with a chemical signature of the tumor that is targeted for destruction.
The first of the three immune stimulants is a drug called leukine (also known as GM-CSF), which summons millions of dendritic cells, key immune cells, to enter the implant. The second is DNA that mimics viral and bacterial DNA and sends a danger signal that activates these cells. The third ingredient is the personalized part of the recipe: a combination of proteins made from the patients’ own tumor. It gives the dendritic cells the unique signature of that person’s tumor, which they share with the warrior T-cells. The “educated” T-cells are then primed to hunt and obliterate the tumor.
The team tested their vaccine implant in mice with melanoma. Control mice that were given implants without the vaccine material died from their cancers within 25 days. Mice that received one vaccine implant showed slower tumor growth, some tumor regression, and survived longer. Of the mice that received two vaccine implants, half completely eliminated all tumors. No other cancer vaccine to date has shown such an effective anti-tumor response.
And now, four short years later, a human trial has started. (Usually it takes about 10 years to move research from animals in labs to human patients.) It’s a Phase I trial—meaning it’s testing for safety in a small group of patients. Each participant will receive four implants over the course of four months. If this trial shows the implant is safe, further trials will be conducted on larger numbers of patients to determine its efficacy—not just in mice, but in humans.
The researchers hope that, like vaccines that confer long lasting immunity to infectious diseases, this new vaccine may endow patients with resistance that keeps the cancer from coming back. That would be an enormous breakthrough—for patients with melanoma, and perhaps for the treatment of many other cancers, too.
References:
[1] In situ regulation of DC subsets and T cells mediates tumor regression in mice. Ali OA, Emerich D, Dranoff G, Mooney DJ. Sci Transl Med. 2009 Nov 25;1(8):8ra19
[2] Infection-mimicking materials to program dendritic cells in situ. Ali OA, Huebsch N, Cao L, Dranoff G, Mooney DJ. Nat Mater. 2009 Feb;8(2):151-8.
Links:
Clinical Trial Site for Melanoma Vaccine (ClinicalTrials.gov)
Cancer Vaccines (NCI factsheet)
NIH support: National Institute of Dental and Craniofacial Research; National Center for Research Resources; National Center for Advancing Translational Sciences

Is there a vaccine for prostate cancer post-radical surgery and radiation therapy?
Thank You for sharing!